Navigating the Holidays with Dual Diagnosis: Practical Strategies for Recovery
The holidays bring together emotional, social, and logistical stressors that can raise relapse risk for people living with both substance use and mental health disorders. More gatherings, greater exposure to alcohol, altered daily routines, and strained family dynamics can interact with anxiety or depression to intensify cravings and reduce coping capacity. Research links seasonal mood shifts and stress with increased substance-related incidents in December and January, and clinicians frequently identify financial pressure and loneliness as common triggers. Spotting these risk areas early helps you prioritize planning and reach out for help if warning signs appear.
How Holiday Triggers Affect Addiction and Mental Health
Holiday triggers increase stress reactivity by engaging the brain’s reward and stress circuits, which can make cravings stronger and prompt impulsive coping. Emotions like grief or loneliness raise cortisol and negative mood, and for some people alcohol or drugs can feel like short-term relief, reinforcing the cycle. With a dual diagnosis, anxiety or depression can blunt self-regulation and heighten sensitivity to cues, creating a feedback loop between substance use and worsening mental health. Quick self-checks are useful: Has your sleep or appetite changed? Are cravings more frequent or intense? Noticing these shifts early makes it easier to use coping skills or seek professional care.
Why Integrated Dual Diagnosis Care Matters Over the Holidays
Integrated dual diagnosis treatment reduces holiday risk by coordinating mental health and addiction care so relapse prevention plans align with emotional triggers and real-world social situations. This approach blends psychotherapy, medication management when appropriate, and structured relapse planning to avoid gaps that can appear when services are fragmented. Evidence shows combined treatments improve symptom stability and lower relapse compared with siloed care, especially when clinicians build anticipatory plans for seasonal stressors. If warning signs persist, such as stronger cravings, worsening mood, or loss of function, early clinical assessment and a coordinated care response can prevent holiday-related harm.
Coping Strategies That Support Recovery During the Holidays
Effective holiday coping combines proactive planning, steady daily routines, and reliable social supports to limit exposure to triggers and strengthen relapse prevention. Planning means identifying high-risk situations, naming a trusted contact, and creating clear exit strategies for gatherings. These steps reduce uncertainty and increase control. Daily anchors such as regular sleep, balanced meals, and scheduled movement protect mood and lower physiological stress that fuels craving.
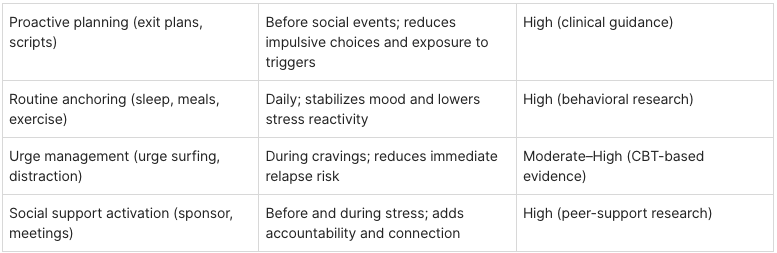
Different strategies fit different moments during the season. Proactive planning like exit plans and scripts works best before social events to reduce impulsive choices and exposure to triggers. Routine anchoring through consistent sleep, meals, and exercise provides daily stabilization of mood and lowers stress reactivity. Urge management techniques such as urge surfing and distraction help during cravings to reduce immediate relapse risk. Social support activation through sponsors and meetings adds accountability and connection before and during stressful times.
These approaches work best together. Planning reduces exposure, routines build resilience, and urge management plus social support handle acute moments.
Practical Techniques to Manage Holiday Stress and Cravings
Practical techniques turn coping strategies into short, repeatable actions that lower cravings and protect recovery when you’re under pressure. Urge surfing helps you notice cravings as passing sensations while using steady breathing and grounding to let them pass. Practiced boundaring boundary scripts and agreeing on exit plans makes to leave difficult situations calmly. Quick distractions like calling a support person, taking a ten-minute walk, or sipping water while focusing on your breath can reduce urge intensity and buy time for clearer choices. These micro-skills work best when rehearsed in advance and stored in a written holiday relapse prevention plan you can consult in the moment.
A simple action plan might include writing an event plan that notes likely triggers, a clear exit, and a go-to support person. Rehearse boundary scripts and exit lines ahead of gatherings to lower on-the-spot stress. Use urge surfing and deep breathing when cravings arrive to reduce physiological arousal. Keep routine anchors like sleep, meals, and movement steady in the days around events. Activate support quickly if warning signs grow worse by calling your sponsor, therapist, or crisis contact.
How Self-Care and Routine Support Stability in Recovery
Daily self-care and predictable routines create biological and psychological anchors that offset holiday unpredictability and support long-term recovery. Habits such as consistent sleep and wake times, nourishing meals, short morning movement, and brief mindfulness or journaling lower stress hormones and improve emotion regulation. Reducing exposure to alcohol-focused social media and scheduling device-free time limits cue-driven cravings and protects reflection. Setting realistic expectations and accepting that not every moment will be joyful reduces shame and allows kinder self-management. Together, these practices create an internal steadiness that makes it less likely temporary stressors will trigger relapse.
How Dunham House’s Dual Diagnosis Care Supports Holiday Recovery
Dunham House offers integrated residential and outpatient dual diagnosis programs that combine evidence-based therapies with experiential modalities to address holiday-specific relapse risk. Our centre provides a one-month intensive stabilization program, a six-month core residential program, and outpatient services.
Each is designed to align mental health treatment with addiction care so seasonal stressors are anticipated and managed. The campus’s peaceful, natural setting and English-language programming help reduce sensory overload that can happen during holidays. Clinicians create individualized relapse prevention plans that include coping rehearsals, family coordination, and community re-engagement strategies tailored to the season.
We blend cognitive and behavioral therapies with group work and experiential methods to target mood symptoms and substance-related triggers that arise at the holidays. Evidence-based approaches such as cognitive behavioral therapy and dialectical behavior therapy teach emotion regulation, distress tolerance, and reframing of trigger-linked thoughts. Group therapy builds peer accountability and provides a place to rehearse social scenarios. Clinicians fold relapse prevention planning into sessions that address holiday-specific cues, creating concrete steps like identifying high-risk relatives and scheduling sober alternatives.
Equine-assisted learning at Dunham House uses interactions with horses to build emotional regulation, clear boundary-setting, and nonverbal communication. These are skills that transfer directly to tense holiday conversations. Working with horses rewards calm, consistent signals and boundaries, which can be practiced and then applied at family meals or gatherings. When combined with CBT and group work, equine sessions form a complementary package that strengthens coping during the festive season.
How Families Can Support Loved Ones in Recovery Over the Holidays
Family involvement is a strong protective factor when it focuses on education, clear boundaries, and structured support rather than rescuing or enabling. Families who learn about dual diagnosis can better see how stressors interact with mental health and substance use, allowing them to respond supportively without taking over. Practical steps like planning conversations in advance, agreeing on nonjudgmental language, and setting emergency contingency plans reduce uncertainty and create a predictable environment for the person in recovery.
Effective communication pairs validation with firm limits, using brief, rehearsed lines that prevent escalation at family gatherings. Examples include calm refusals like “I care about you, and I can’t support drinking in my home” and simple boundary statements like “I will leave if alcohol is served.” These are less likely to provoke argument when delivered steadily. Prepare conversations in advance, keep statements short, and focus on behaviors rather than character. Avoid lecturing, shaming, or making unenforceable ultimatums.
Family support lowers holiday stress by adding structure, watching for early warning signs, and reinforcing treatment-consistent choices in real time. Informed family members can prompt coping skills, help implement exit strategies during gatherings, and assist with tasks that reduce pressure like shared meal planning or arranging rides. A simple family-supported holiday plan might assign roles. One person observes triggers, another ensures the individual has a quiet space if overwhelmed, and a third is the designated transport contact. This builds a safety net that lowers crisis risk.
Sober Holiday Activities and Community Resources That Support Recovery
Volunteering to connect with the community and counter isolation.
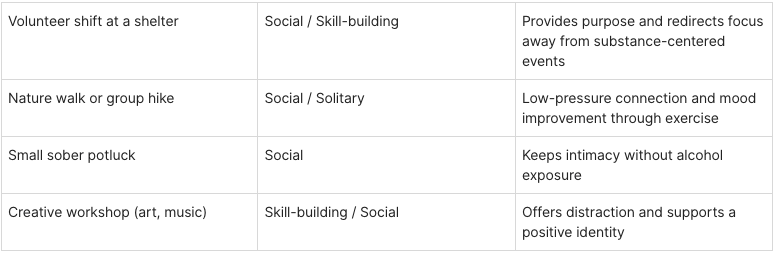
Sober activities and community connections replace high-risk gatherings with meaningful alternatives that offer belonging without substance exposure. Purposeful events like volunteering, outdoor outings, creative workshops, and small sober potlucks provide social contact, skill-building, and mood-boosting experiences that counter isolation. Community resources such as peer support meetings, online recovery groups, and organized volunteer programs give steady social reinforcement and reduce the sense of facing the season alone.
Intentional sober celebrations create new traditions that replace alcohol-centered rituals and build recovery-supportive memories. Consider a neighborhood volunteer morning, a themed sober potluck with close friends, a nature outing, a group creative or cooking session, or a small game night with agreed substance-free rules. When organizing, keep guest lists small and supportive, communicate boundaries in advance, and choose activities that naturally occupy attention and spark conversation.
Building community creates a protective social identity that reduces isolation and boosts accountability during the holidays. Peer support groups and recovery communities share practical strategies and norms that normalize sobriety at celebrations and provide quick access to emotional support when stressors arise. Making community involvement part of your holiday plan can turn an isolating season into one of steady social reinforcement.
Conclusion
Navigating the holiday season in recovery requires understanding the unique challenges and using practical, evidence-informed strategies. By planning ahead, keeping routines steady, and leaning on trusted supports, you can reduce relapse risk and protect your wellbeing. Engaging in sober activities and strengthening community ties further builds resilience during this time. For tailored support and more resources, explore Dunham House’s programs or contact our admissions team to discuss options that fit your recovery journey.
Dunham House
About Dunham House
Located in Quebec's Eastern Townships, Dunham House is a residential treatment centre specializing in addiction and providing support to individuals with concurrent mental health challenges. We are the only residential facility of our kind in Quebec that operates in English.
Our evidence-based programs include a variety of activities such as art, music, yoga, and equine-assisted therapy. In addition to our residential services, we offer a full continuum of care with outpatient services at the Queen Elizabeth Complex in Montreal.