What Are the Key Factors Contributing to Homelessness and How Can They Be Addressed?
Homelessness is a complex social condition marked by the absence of stable, safe, and adequate housing, driven by intersecting factors like mental illness, substance use, poverty, and systemic policy gaps. This article explains how these factors operate, why they increase risk, and which integrated clinical and housing responses reduce it. Readers will learn about mental health disorders and substance use patterns linked to housing instability, how economic and housing market dynamics amplify vulnerability, and the importance of trauma-informed, dual-diagnosis care for prevention. The piece maps evidence-based therapies, system-level prevention strategies, and local resources relevant to Canada and Quebec, emphasizing actionable understanding and program models that improve housing outcomes.
What Mental Health Challenges Contribute to Homelessness?
Mental health challenges contribute directly to homelessness by producing functional impairments that undermine income, relationships, and tenancy. Severe mental illnesses and common mood disorders disrupt daily living, reduce employment capacity, and increase service disengagement, making housing loss more likely. Early access to treatment, continuity of care, and community-based supports reduce these risks by restoring functioning and stabilizing routines. Subsections examine specific disorders, mechanisms, trauma links, and preventive treatment models.
Which Mental Health Disorders Are Most Linked to Housing Instability?
Severe mental illnesses like schizophrenia, psychotic disorders, major depressive disorder, bipolar disorder, and PTSD are frequently implicated in housing instability. These disorders often involve cognitive, emotional, or behavioral symptoms that impair decision-making, work performance, and ability to meet rental obligations. Stigma and discrimination limit employment and rental access; episodic crises can precipitate income loss or eviction. Stable outpatient supports and assertive community treatment reduce rapid transitions to homelessness.
How Does Mental Illness Increase the Risk of Becoming Homeless?
Mental illness increases homelessness risk through multiple pathways: symptom-driven job loss, breakdown of social supports, difficulty navigating benefit systems, and treatment disengagement. Financial instability follows when symptoms reduce work capacity or hospitalizations interrupt employment, creating rent arrears and housing insecurity. Cognitive symptoms hinder medication adherence, weakening relationships with landlords and service providers. Integrated case management linking clinical stabilization with income supports and tenancy assistance prevents eviction spirals.
What Role Does Trauma and PTSD Play in Mental Health and Homelessness?
Trauma and PTSD operate as antecedents and perpetuating factors for homelessness by increasing vulnerability to mood disorders, substance use, and social isolation. Traumatic histories from childhood abuse to community violence can create persistent hyperarousal, avoidance, and difficulty trusting services, complicating engagement with housing and clinical supports. PTSD symptoms often co-occur with depression and substance use as coping responses, compounding housing loss risk. Trauma-informed approaches prioritizing safety, choice, and empowerment improve retention in care and reduce re-traumatization.
Trauma-Informed Care for Homelessness: Addressing Mental Illness, Substance Use Disorders, and Trauma
Many individuals experiencing homelessness have severe mental illness, chronic substance use disorders, and extensive trauma histories. To mitigate these effects, homelessness service settings adopt trauma-informed care (TIC) approaches. TIC delineates core principles, analyzes implementation impediments, and emphasizes strategies for overcoming barriers. (C Bransford, 2019)
How Can Mental Health Treatment Prevent Homelessness?
Evidence-based mental health treatments prevent homelessness by restoring functioning, improving symptom management, and linking clinical care to practical supports like employment and housing navigation. Early intervention programs, community mental health teams, and integrated outpatient services enhance continuity and reduce crisis-driven displacement. Combining psychotherapy, medication management, and social support helps stabilize income and tenancy; outreach models reconnect those disengaged from care. Embedding housing casework within clinical teams ensures mental health improvements translate into durable housing outcomes.
How Does Addiction Influence the Causes and Persistence of Homelessness?
Addiction contributes to both the onset and persistence of homelessness by eroding finances, straining relationships, and reducing engagement with services. Substance use disorders increase eviction risk when funds are diverted from housing costs, behaviors jeopardize tenancy, and legal or health crises force housing exits. Homelessness itself raises the likelihood of substance use as a coping strategy, creating a bidirectional relationship that sustains instability. Effective interventions require integrated treatment models addressing substance use alongside co-occurring mental health conditions to interrupt these reinforcing cycles.
What Types of Substance Use Disorders Are Common Among Homeless Populations?
Alcohol use disorder, opioid use disorder, and stimulant use disorders are common among people experiencing homelessness, each bringing distinct harms and treatment needs. Alcohol's ubiquity often makes it a prevalent substance and a major driver of medical complications and tenancy breaches. Opioids increase overdose risk and complicate housing program engagement. Stimulant use can heighten behavioral volatility and interfere with routines necessary to maintain housing. Tailored interventions must account for substance-specific risks and social contexts.
How Does Addiction Lead to Housing Instability and Homelessness?
Addiction leads to housing instability by draining income, provoking eviction-worthy behaviors, fracturing family/social supports, and creating legal entanglements. Diverting financial resources to substance purchase produces rent arrears and utilities issues; substance-related behaviors can violate lease terms or generate complaints. Criminalization and incarceration create abrupt housing loss and complicate re-entry. Breaking these pathways requires integrated supports combining harm reduction, income stabilization, legal assistance, and clinical care to protect tenancies during recovery.
Why Is Integrated Dual Diagnosis Treatment Essential for Recovery?
Integrated dual diagnosis treatment—addressing mental health and substance use concurrently is essential because co-occurring conditions interact to increase relapse risk and destabilize housing. When treated separately, conflicting plans and care gaps leave individuals vulnerable to symptom recurrence. Integrated models coordinate psychotherapy, medication-assisted treatment, relapse-prevention planning, and social supports under a unified plan, reducing readmission, supporting tenancy, and improving long-term recovery. Concurrent care is a cornerstone of homelessness prevention for co-occurring disorders.
How Does Addiction Relapse Affect Homelessness Risk?
Relapse often triggers immediate threats to housing stability by reigniting behaviors that undermine tenancy, eroding income, and distancing individuals from supports. A single relapse can lead to missed rent payments, eviction notices, or family breakdown; repeated relapses compound vulnerability. Recognizing relapse as part of a chronic disease model emphasizes rapid re-engagement strategies, relapse-prevention plans tied to housing assistance, and flexible supports to prevent eviction during setbacks. Continuity of care and crisis-response pathways reduce the chance relapse leads inevitably to homelessness.
What Economic and Housing Factors Drive Homelessness?
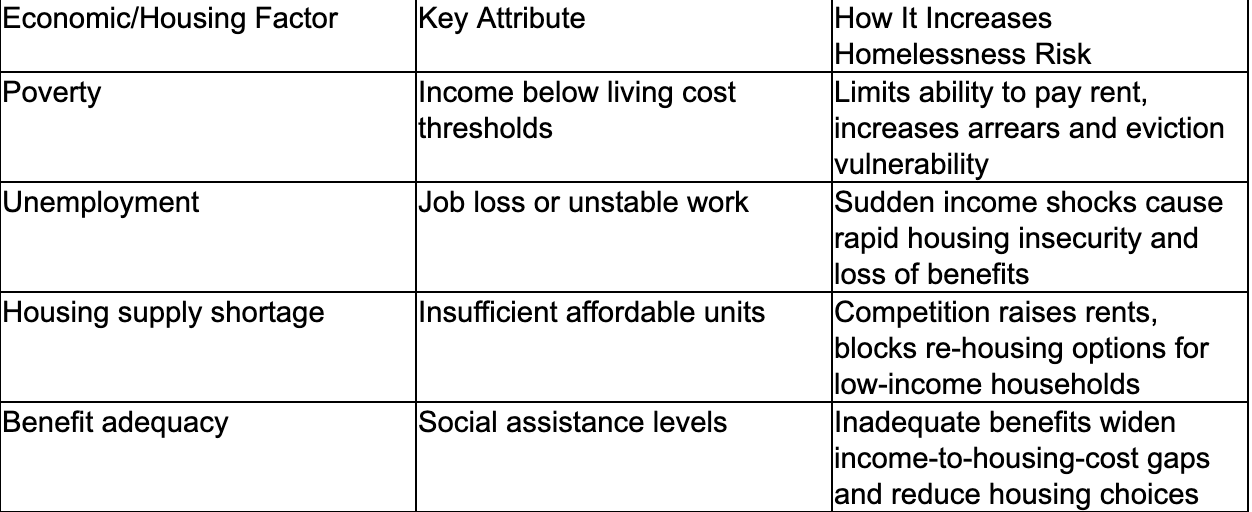
Poverty, unemployment, and a shortfall of affordable housing are primary economic drivers elevating homelessness risk by creating a persistent gap between income and housing costs. When wages, benefits, or employment are insufficient to cover rising rents, households become precarious and more likely to lose housing after shocks. These economic drivers interact with mental health and addiction to produce compounded risk: limited income reduces treatment access, and unstable housing worsens clinical outcomes. The following table clarifies how each factor contributes to homelessness risk in Canada and Quebec.
The table below compares economic and housing factors, their core attributes, and their influence on homelessness risk:
This comparison shows that economic insufficiency and supply-side shortages directly erode housing security and must be addressed alongside clinical supports to reduce homelessness.
How Do Poverty and Unemployment Increase Homelessness Risk?
Poverty and unemployment increase homelessness risk by removing the financial buffer that prevents shortfalls from translating into housing loss. Low-income individuals and families have minimal savings, so even brief unemployment or reduced hours can lead to missed rent and eviction. Benefit systems not covering regional housing costs exacerbate this, and precarious work increases exposure to shocks. Strengthening income supports, improving job stability programs, and linking employment services to housing assistance create buffers that reduce transitions into homelessness.
Why Is Lack of Affordable Housing a Critical Factor?
Lack of affordable housing is critical because it constrains options for low-income households and makes exits from homelessness slower and less probable. When affordable units are scarce, competition forces people to accept substandard or unstable arrangements vulnerable to displacement. Landlords may screen out those with complex needs; waitlists for subsidized housing can be long, prolonging instability. Increasing supply and targeted allocations for people with mental health and addiction needs improve housing retention and reduce system pressure.
How Do Housing Market Challenges Affect Mental Health and Addiction?
Housing market stressors frequent moves, overcrowding, and threat of eviction worsen mental health symptoms and increase reliance on substances as coping mechanisms. Chronic insecurity elevates anxiety, depression, and trauma symptoms; unstable housing disrupts treatment adherence and recovery routines. Homelessness and poor housing conditions expose people to environments that normalize substance use. Integrating housing stabilization with clinical care reduces stressors and supports sustained recovery.
What Are the Social Determinants of Health Related to Homelessness?
Social determinants like income, education, social inclusion, and healthcare access shape homelessness risk by influencing resilience and resource access. Low educational attainment and limited social capital impede employment and service navigation, while systemic discrimination intensifies vulnerability for marginalized groups. Interventions addressing these determinants education supports, inclusive housing policies, and equitable health access reduce structural drivers of homelessness and improve recovery prospects when paired with targeted clinical programs.
How Do Trauma and Domestic Violence Contribute to Homelessness?
Trauma and domestic violence are immediate and powerful causes of homelessness, often forcing people to flee unsafe environments and creating long-term barriers to re-housing. Survivors may prioritize safety over affordability, leading to crowded or temporary housing arrangements lacking security. Trauma also increases co-occurring mental health and substance use disorders, complicating access to stable housing and services. Trauma-informed responses in housing and clinical settings play a central role in preventing and resolving homelessness.
What Is the Impact of Domestic Violence on Housing Stability?
Domestic violence often results in immediate displacement when individuals leave to escape danger, creating urgent needs for shelter and long-term housing solutions. Survivors may lose rental history or face financial setbacks impeding new housing; safety concerns can limit acceptable options. Legal barriers, lack of accessible shelters, and confidentiality issues further complicate re-housing. Coordinated legal aid, dedicated housing pathways, and survivor-centered supports reduce the duration and recurrence of homelessness following domestic violence.
How Does Trauma Lead to Co-occurring Mental Health and Addiction Issues?
Trauma can precipitate both mental health disorders and substance use as coping strategies, leading to co-occurring conditions that heighten homelessness risk. Chronic trauma dysregulates stress responses and can drive self-medication behaviors, increasing dependency and complicating clinical courses. These co-occurring conditions interact to reduce treatment engagement and vocational functioning, making housing retention more difficult. Integrated, trauma-informed treatment that treats trauma alongside mental health and addiction supports better stabilization and housing outcomes.
Why Is Trauma-Informed Care Vital in Preventing Homelessness?
Trauma-informed care is vital because it reduces re-traumatization, increases trust, and improves engagement with services key elements for securing and maintaining housing. Principles such as safety, transparency, choice, and empowerment create environments where survivors can participate in planning and recovery. Embedding trauma-informed practices into housing programs and clinical services increases retention, supports tenancy, and reduces the chance that unresolved trauma will lead to service disengagement and housing loss.
What Systemic Failures and Social Issues Perpetuate Homelessness?
Systemic failures fragmented services, policy misalignment between health and housing sectors, and underfunded supports perpetuate homelessness by leaving people without coordinated pathways from crisis to stability. Historical policies like deinstitutionalization without parallel community investment contributed to gaps in continuity of care; structural inequalities concentrate risk among marginalized populations. Addressing these systemic issues requires cross-sector reforms, integrated service pathways, and targeted investments to create sustainable prevention and rehousing mechanisms.
How Do Inadequate Social Services and Policy Gaps Affect Homelessness?
Inadequate social services and policy gaps produce service fragmentation where individuals must navigate multiple uncoordinated systems to secure housing, income, and health care. This fragmentation increases drop-off rates and delays interventions until crises occur. Policy mismatches like separate eligibility rules for housing and clinical services prevent seamless transitions and undermine prevention. Creating integrated referral systems, shared data protocols, and joint funding models helps align services around person-centered outcomes that reduce homelessness risk.
What Role Does Deinstitutionalization of Mental Health Patients Play?
Deinstitutionalization without sufficient community-based supports historically increased homelessness risk by discharging people from hospitals without appropriate housing or outpatient care. This involves abrupt loss of institutional supports and insufficient community infrastructure to absorb clinical and social needs. Rebuilding robust community mental health systems with housing-linked services and supported transitions reduces the likelihood that hospital discharge becomes a pathway to homelessness.
How Does Racial Inequality Influence Homelessness Rates?
Racial inequality influences homelessness rates through structural mechanisms that limit access to housing, income, and services for Indigenous and racialized communities. Historical dispossession, discrimination in employment and housing markets, and culturally inappropriate services result in disproportionate representation among homeless populations. Culturally informed, community-led responses and policy measures addressing systemic exclusion are essential to reduce these disparities and provide effective prevention and rehousing pathways.
What Are Effective Prevention Strategies at the System Level?
Effective prevention strategies include housing-first approaches, integrated health and housing services, income supports calibrated to local housing costs, and policy reforms expanding affordable supply. Cross-sector coordination linking healthcare, social services, and housing agencies—creates continuity that prevents people from falling through cracks. Investment in early intervention, eviction prevention programs, and targeted supports for people with co-occurring disorders reduces system pressure and leads to better long-term outcomes.
Effectiveness of Housing First for Homeless Individuals with Mental Illness: Service Utilization Patterns
Housing First effectively provides stable housing and modifies service utilization for many homeless individuals with mental illness. Research investigated changes in service utilization among individuals with mental illness receiving Housing First versus standard care, and how patterns varied between those who achieved stable housing and those who did not. (N Kerman, 2018)
How Does Dual Diagnosis Treatment Address the Root Causes of Homelessness?
Dual diagnosis treatment integrated care for co-occurring mental health and substance use disorders addresses root causes of homelessness by treating interacting conditions that together destabilize housing. Coordinated clinical plans, relapse-prevention strategies, and social support linkages reduce symptoms leading to job loss and tenancy breaches. Integrated approaches improve engagement with housing services and enable tailored aftercare that supports long-term stability. The following table compares program types commonly used to prevent homelessness through dual-diagnosis care.
This table compares residential and outpatient program types, their focus, intensity, and suitability for preventing homelessness:
Comparing these models clarifies that program duration and intensity should match the complexity of co-occurring disorders to best support housing retention and prevent recurrent homelessness.
What Is Dual Diagnosis and Why Is It Critical for Homeless Individuals?
Dual diagnosis refers to the co-occurrence of substance use disorders alongside mental health disorders, critical for homeless individuals because these conditions interact to magnify functional impairment and relapse risk. Treating both concurrently reduces contradictory treatment plans and fills care gaps that otherwise lead to cycles of relapse and housing loss. Concurrent treatment stabilizes symptoms, enhances adherence to tenancy obligations, and supports reintegration into employment and social networks that sustain housing.
How Does Dunham House Provide Integrated Care for Co-occurring Disorders?
Dunham House, a non-profit residential treatment center in Quebec's Eastern Townships, specializes in dual diagnosis care, offering one-month and six-month residential options plus outpatient services. Programs combine evidence-based therapies ,traditional clinical and holistic modalities, delivered by compassionate, highly trained staff on an 85-acre nature campus. English-language programming and flexible program lengths match intensity to individual needs, supporting stabilization, relapse prevention, and transitions back to community housing. These integrated attributes help translate clinical gains into improved housing stability by pairing therapeutic progress with skills-building and aftercare planning.
What Evidence-Based Therapies Support Recovery from Homelessness?
Evidence-based therapies for dual diagnosis include cognitive-behavioral therapy, trauma-informed modalities, relapse-prevention planning, and supportive psychosocial interventions addressing housing and occupational skills. CBT targets maladaptive thoughts and behaviors; trauma-informed therapies resolve underlying drivers of substance use and mental health symptoms. Relapse-prevention approaches and peer-supported recovery help maintain tenancy by creating practical strategies for stress and cue management. Holistic supports like nature-based and experiential therapies enhance engagement and complement clinical treatments to foster durable recovery and housing retention.
How Does a Healing Environment Enhance Treatment Outcomes?
A healing environment characterized by safety, natural settings, and community supportenhances treatment outcomes by reducing stress, improving sleep/mood, and increasing engagement in therapy. Nature-rich campuses and supportive residential communities promote routine, social connectedness, and opportunities to build daily living skills essential for sustaining housing. For people exiting homelessness, such environments provide a stable setting to practice tenancy-related behaviors and develop relapse-prevention strategies before reintegration. Embedding therapeutic activities within a restorative setting strengthens resilience for long-term housing.
Homelessness, Housing Instability, and Mental Health: A Global Perspective and Interventions
This review examines the bidirectional relationship between mental health and homelessness globally, highlighting structural factors contributing to housing instability and its mental ill-health consequences. It discusses local, national, and international initiatives, including Housing First, and strategies for healthcare professionals to act as agents of change, emphasizing the fundamental importance of housing to mental health. (2020)
What Are the Pathways to Preventing Homelessness Through Mental Health and Addiction Support?
Preventing homelessness requires early intervention, family/community supports, accessible dual-diagnosis programs, and coordinated resource pathways connecting clinical care to housing. Rapid access to screening and treatment reduces crisis-level symptoms precipitating eviction, while family-inclusive practices and community resources build social capital supporting tenancy. Integrated aftercare and outpatient continuity following residential treatment maintain gains and reduce relapse-linked housing loss. The following list outlines practical prevention pathways.
Key prevention pathways include:
Rapid screening and early access to mental health and addiction services to intercept escalating needs before housing loss occurs.
Housing-focused case management that links clinical treatment with rent supports, eviction prevention, and landlord mediation.
Family education and community-based supports that strengthen social networks and reduce isolation.
Aftercare and outpatient continuity that provide sustained relapse prevention and tenancy support following residential care.
These pathways emphasize coordinated, timely interventions that pair clinical stabilization with practical housing supports. Subsections explore early intervention, family roles, program access, and authoritative resources in the Canadian and Quebec context.
How Can Early Intervention Reduce Homelessness Risk?
Early intervention reduces homelessness risk by identifying symptoms and substance use early, offering rapid access to treatment, and connecting clients with housing supports before crises escalate. Screening in primary care, emergency departments, and community settings allows prompt referral to integrated programs that stabilize symptoms and secure tenancy. Supported housing placements and short-term rent assistance during treatment bridge gaps that otherwise lead to eviction. Embedding housing navigators in clinical teams ensures clinical improvement translates into durable housing outcomes.
What Role Do Family and Community Support Systems Play?
Family and community supports play a protective role by providing emotional backing, practical assistance with daily tasks, and help navigating systems for benefits and housing. Family-inclusive practices, family therapy, education on relapse prevention, and involvement in discharge planning improve retention and reduce recurrence of homelessness. Community organizations, peer networks, and faith-based groups offer social capital and informal supports that often make the difference between temporary crises and prolonged housing loss. Strengthening these networks increases resilience and fosters sustainable reintegration.
How Can Access to Dual Diagnosis Programs Improve Long-Term Stability?
Access to dual-diagnosis programs—both residential and outpatient improves long-term stability by delivering coordinated treatment, relapse prevention, and life-skills training tailored to co-occurring conditions. Residential programs provide intensive stabilization and skill-building, while outpatient services offer continuity and support during reintegration into housing and work. Aftercare plans including housing case management, community follow-up, and peer support reduce relapse and preserve tenancy. Ensuring program availability and flexible admission pathways increases the likelihood that people at risk receive the right level of care at the right time.
What Are Key Resources and Services Available in Quebec and Canada?
Authoritative national and provincial resources provide data, policy guidance, and service directories for homelessness, mental health, and addiction, supporting prevention and intervention planning. Organizations focused on homelessness research, government statistics, addiction and mental health policy, and provincial service directories offer evidence and referral pathways. Local community agencies and peer-support networks complement these resources by providing on-the-ground assistance and navigation. Consulting these hubs helps align clinical interventions with available housing and social supports in Canada and Quebec.
For those seeking integrated residential care that targets co-occurring disorders, Dunham House offers structured program options including short-term (one-month) and core (six-month) residential pathways along with outpatient services. Their programs combine evidence-based therapies with holistic elements on an expansive nature campus and are delivered in English by compassionate teams. Individuals and families considering dual-diagnosis treatment may find such integrated models helpful for stabilizing symptoms, preventing relapse, and supporting transitions back to community housing.
Early Treatment Access: Rapid referral pathways prevent crisis-driven housing loss.
Integrated Care Models: Concurrent treatment of mental health and addiction lowers relapse and tenancy risk.
Reinsertion Programs: These programs help residents with their housing options after treatment, providing support to transition successfully back into the community.
These combined strategies illustrate how clinical, social, and housing interventions work together to prevent homelessness.
Conclusion
Addressing the multifaceted causes of homelessness through integrated mental health and addiction support is essential for fostering long-term stability. By implementing early intervention strategies and dual-diagnosis treatment, we can significantly reduce the risk of housing loss and improve overall well-being. Engaging with community resources and tailored programs enhances the effectiveness of these interventions, ensuring that individuals receive the comprehensive care they need. For more information on how to access these vital services, discover how Dunham House can support your journey to recovery.
Dunham House
About Dunham House
Located in Quebec's Eastern Townships, Dunham House is a residential treatment centre specializing in addiction and providing support to individuals with concurrent mental health challenges. We are the only residential facility of our kind in Quebec that operates in English.
Our evidence-based programs include a variety of activities such as art, music, yoga, and equine-assisted therapy. In addition to our residential services, we offer a full continuum of care with outpatient services at the Queen Elizabeth Complex in Montreal.