Navigating Persistent Discomfort: Key Factors and Integrated Care
Persistent discomfort, often lasting beyond three months, is more than just a lingering ache. It arises from a complex interplay of physical and emotional elements that can keep you trapped in a cycle of pain and limit your daily life.
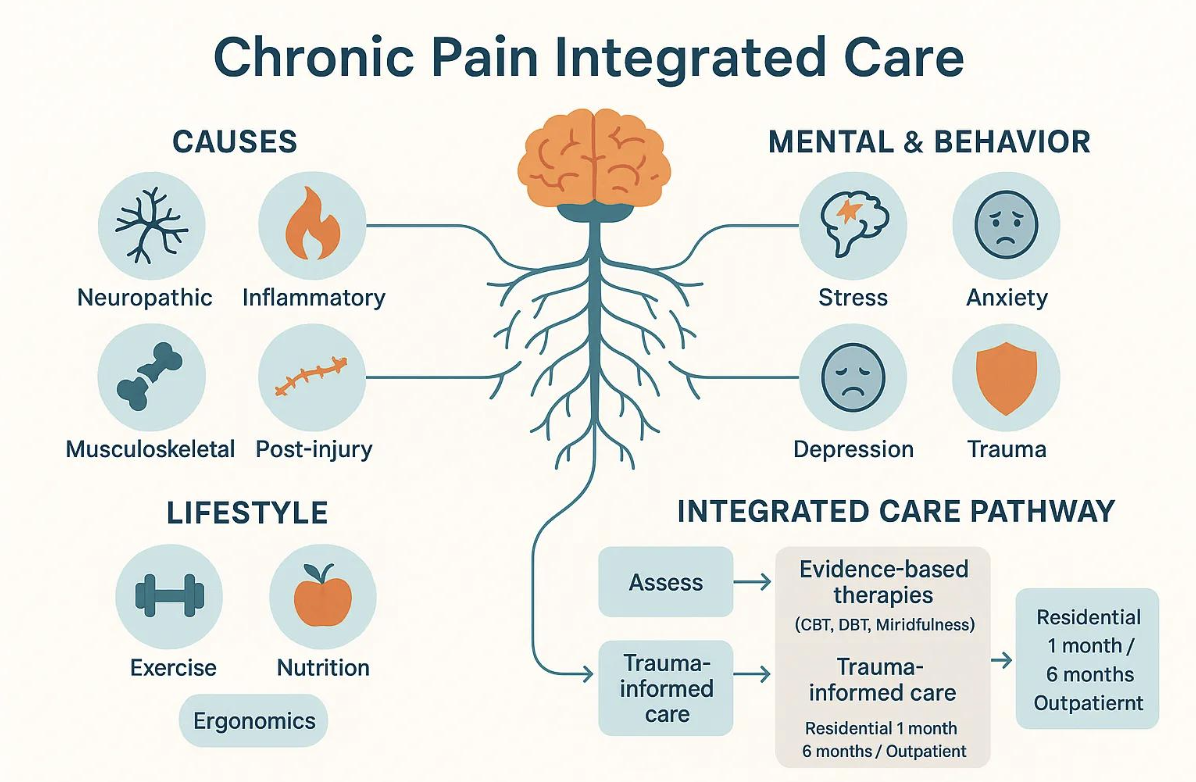
This guide dives into the roots of ongoing discomfort, exploring how physical issues like nerve damage and inflammation, alongside emotional factors such as stress and past trauma, can amplify your pain. We'll differentiate between nerve-related and tissue-related pain, look at lifestyle risks, and introduce holistic ways to cope. We'll also examine the deep connection between pain, mental well-being, and substance use, outlining how to manage dual diagnoses in various settings. Finally, we'll discuss integrated programs that blend proven therapies with holistic approaches to help reduce reliance on opioids and foster lasting improvements.
What's Behind Chronic Pain?
Persistent discomfort often stems from ongoing physical processes or nerve injuries, leading to lasting aches and reduced movement. Understanding these core issues is vital for effective treatment, guiding interventions from nerve-focused care to anti-inflammatory or rehabilitative strategies.
Nerve Damage: Injuries to your peripheral or central nerves can lead to ongoing nerve-related symptoms like burning or electric sensations.
Arthritis: Degenerative or inflammatory joint conditions cause persistent tissue-related and inflammatory pain, often limiting your ability to move.
Injury and Surgical Trauma: Structural damage and scar tissue can contribute to ongoing pain even after initial healing.
Inflammation: Systemic or localized inflammatory conditions can keep nerve signals firing and amplify pain signals in your central nervous system.
Musculoskeletal Degeneration: Conditions like disc disease, tendinopathy, and chronic soft-tissue strain can cause long-term pain and disability.
These categories frequently overlap, making a precise assessment essential for targeted interventions and preventing the progression of chronic pain.
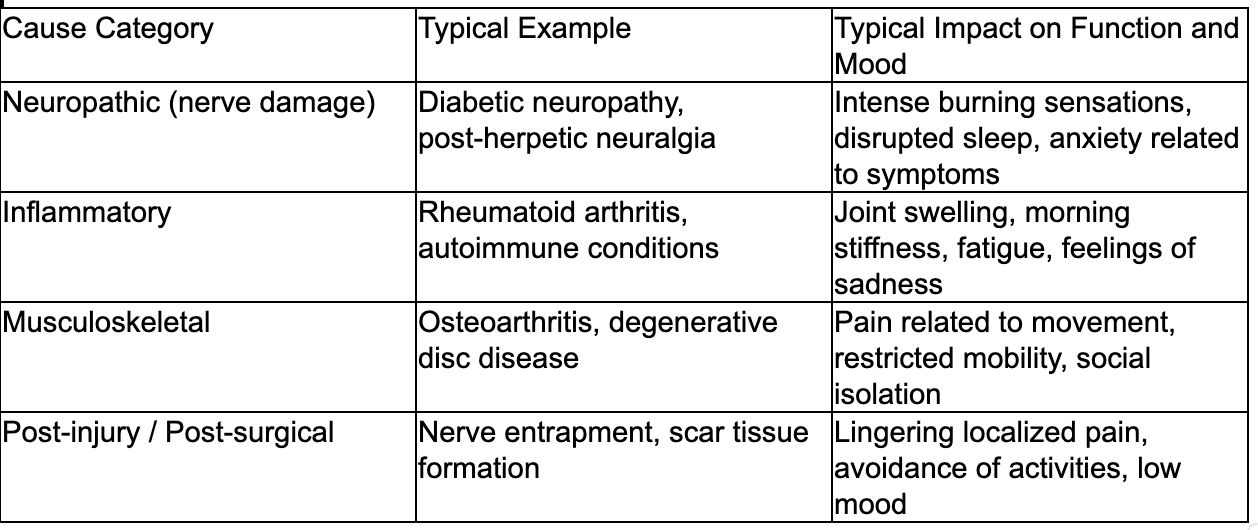
Different physical causes present with distinct clinical patterns. The table below compares major cause types, examples, and their impact on your function and mood.
Identifying the cause influences how we manage your pain and provide psychological support. Next, we'll explore the physiological mechanisms involved.
What Physiological Factors Lead to Persistent Pain?
Persistent pain develops through ongoing nociception (pain signaling), peripheral sensitization (overly sensitive pain receptors), and central sensitization (amplified pain signals in the spinal cord and brain). These processes lead to heightened sensitivity, allodynia (pain from non-painful stimuli), and pain lingering after tissue healing, disrupting sleep and activity, and increasing disability.
Diabetic neuropathy and degenerative disc disease are examples of how changes in the peripheral and central nervous systems can prolong pain. Recognizing these mechanisms guides pharmacological, rehabilitative, and psychological interventions to reduce signal amplification and restore function.
How Do Neuropathic Pain Causes Differ from Other Types?
Neuropathic pain stems from damage to the somatosensory nervous system, manifesting as burning, shooting, or electric-shock sensations, often with numbness or tingling. This differs from nociceptive/inflammatory pain, which is typically aching, movement-related, and localized. Causes include nerve compression and metabolic disorders, requiring tailored strategies like specific medications or neuromodulation. Accurate identification improves treatment selection and reduces reliance on opioids.
What Role Do Musculoskeletal and Inflammatory Conditions Play?
Musculoskeletal and inflammatory conditions (e.g., osteoarthritis, inflammatory arthritis) generate persistent pain through joint degeneration, tissue overuse, and immune responses. Mechanical stress and inflammation can lead to peripheral and central sensitization, causing widespread symptoms and fatigue. These conditions often limit function and increase the risk of depression and anxiety. Early, comprehensive management combining rehabilitation, anti-inflammatory strategies, and psychosocial support can prevent chronic disability.
How Do Psychological and Emotional Factors Contribute to Chronic Pain?
Psychological and emotional factors significantly influence chronic pain by affecting how your central nervous system processes pain, increasing your focus on sensations, and shaping behaviors that perpetuate disability. These factors can heighten pain intensity, impair coping mechanisms, and increase healthcare utilization. Stress, anxiety (leading to hypervigilance and catastrophizing), and depression (reducing motivation) all contribute to deconditioning and reinforcing pain cycles. Below are key psychological drivers and behavioral approaches to reduce central sensitization and improve functioning.
Cognitive Behavioral Therapy (CBT) for pain: Enhances coping skills and reduces catastrophic thinking about pain.
Dialectical Behavior Therapy (DBT) strategies: Provides tools for managing intense emotions, particularly in complex cases.
Mindfulness and relaxation techniques: Help lower physiological arousal and reduce focus on pain sensations.
Trauma-informed approaches: Address past adverse experiences that may contribute to physical distress and dysregulation.
These clarify treatment targets. Next, we'll examine the connections between stress, mood disorders, and persistent pain.
What Is the Link Between Stress, Anxiety, and Chronic Pain?
Stress and anxiety intensify pain through physiological pathways like HPA axis activation and heightened sympathetic activity, sensitizing neural circuits and increasing muscle tension. Anxiety also fosters avoidance and hypervigilance, limiting beneficial movement. High stress correlates with greater pain persistence and disability. Interventions targeting stress reactivity, such as CBT, structured activity, and relaxation training, can reduce central sensitization and improve outcomes.
How Do Depression and Trauma Influence Persistent Pain?
Depression alters pain perception by weakening pain-inhibiting systems, reducing motivation for activity, and increasing the perception of disability, prolonging impairment. Past trauma can cause neurobiological changes like hyperarousal and amplified sensations, contributing to chronic pain. Trauma-informed care and integrated psychotherapy (e.g., trauma-focused CBT, EMDR) are crucial for preventing re-traumatization and improving engagement in rehabilitation. Screening for depression and trauma is essential for aligned interventions.
What Are Learned Pain Behaviors and Their Impact?
Learned pain behaviors (e.g., guarding, activity avoidance, reassurance-seeking) can reinforce pain by causing deconditioning and limiting beneficial movement. While offering short-term relief, they can increase long-term disability and diminish quality of life.
Behavioral strategies like gradual exposure, pacing, and reinforcing adaptive behaviors can retrain movement and rebuild physical tolerance.
Rehabilitation programs that combine behavioral retraining with physical therapy are effective in reducing disability and supporting a return to meaningful activities.
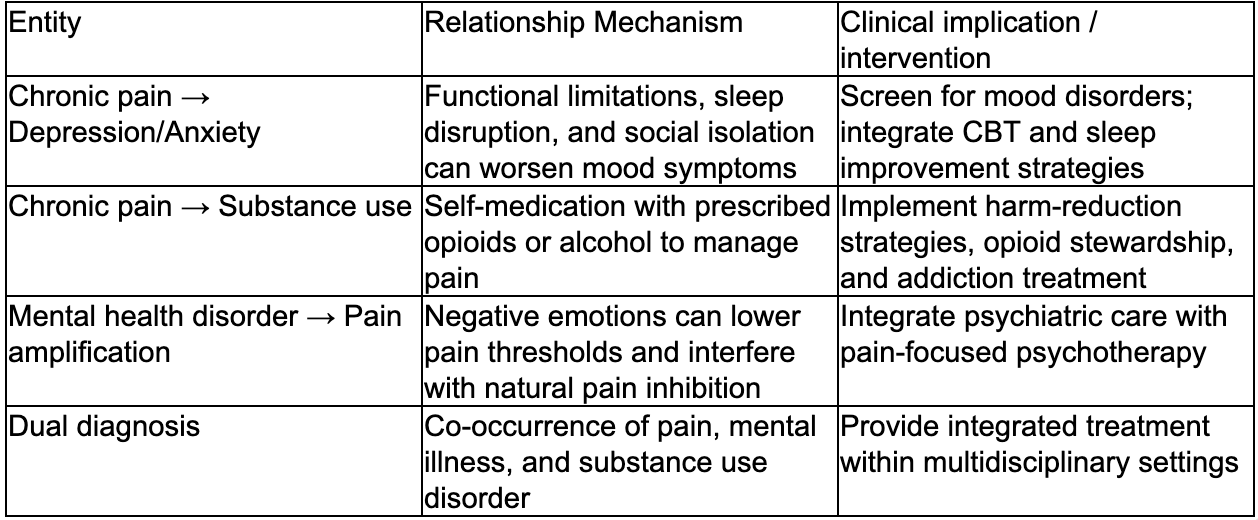
What Is the Connection Between Chronic Pain, Mental Health, and Addiction?
Chronic pain, mental health disorders, and addiction are intricately linked. Pain increases the risk of depression and anxiety, which can, in turn, heighten pain perception. Untreated pain and mood disturbances may lead to substance use. This interconnectedness highlights the importance of screening for depression and substance use in chronic pain management. Integrated treatment addressing pain and addiction concurrently often yields better outcomes. Dual diagnosis management focuses on treating these co-occurring conditions with coordinated medical, psychological, and social resources to minimize harm and improve functioning.
Individuals seeking integrated care for co-occurring pain, mental health, and addiction challenges benefit from combined psychiatric and addiction-focused treatment. Dunham House offers dual-diagnosis programs for addiction and concurrent mental health disorders, utilizing an integrated recovery approach. Our programs include 1-month, 6-month, and outpatient options, emphasizing evidence-based therapies and holistic supports.
How Does Chronic Pain Affect Mental Health Disorders Like Depression and Anxiety?
Chronic pain often causes sleep disturbances, reduced work capacity, and social withdrawal, contributing to depression and anxiety. These mood disorders further sensitize pain pathways. Pain and mood symptoms reinforce each other, so treating one in isolation is often ineffective. Clinical practice requires regular mood disorder screening and coordinated care plans combining pain management, psychotherapy, and medication. Early psychosocial interventions can prevent worsening disability and reduce reliance on high-risk medications.
Can Addiction Develop as a Result of Chronic Pain?
Addiction can develop from prescription opioid exposure, self-medication, and behavioral reinforcement from temporary pain relief. Risk factors include a prior substance use disorder, unmanaged psychiatric conditions, and high pain distress. Opioid prescribing for chronic non-cancer pain increases addiction risk, emphasizing conservative practices and alternative strategies. Harm-reduction approaches (e.g., tapering, naloxone education, concurrent addiction treatment) can mitigate adverse outcomes. Integrated programs treating both pain and addiction simultaneously show better functional and substance-use outcomes.
What Is Dual Diagnosis Treatment for Chronic Pain and Addiction?
Dual diagnosis treatment for individuals living with both addiction and physical pain focuses on comprehensive, integrated care. This approach combines medical support, behavioral therapies such as CBT and DBT, relapse prevention, and rehabilitation strategies within a coordinated framework. Both residential and outpatient settings provide personalized treatment, emphasizing trauma-informed practices to ensure safety and trust. The ultimate goal is to reduce discomfort, support lasting recovery, and improve overall quality of life.
Which Lifestyle and Environmental Factors Increase the Risk of Chronic Pain?
Lifestyle and environmental factors (e.g., prolonged sitting, obesity, poor ergonomics, repetitive movements) increase mechanical/inflammatory stress, accelerate degeneration, and cause deconditioning, sustaining pain. These modifiable risks interact with psychological factors, making lifestyle interventions crucial for chronic pain and dual diagnosis plans. Gradual approaches combining physical activity, improved sleep, and workplace adjustments can reduce risk and support recovery when integrated with behavioral therapy. Below are evidence-supported lifestyle changes for reducing pain and improving function.
Begin graded exercise: Small, progressive increases in physical activity help rebuild tolerance and reduce fear associated with movement.
Enhance sleep hygiene: Consistent, quality sleep supports the body's natural pain-inhibiting systems and mood regulation.
Optimize nutrition and weight: A balanced diet and weight management can reduce inflammation and ease stress on joints.
Improve ergonomics and reduce repetitive strain: Adjustments at work or home can prevent overuse injuries and minimize triggers for pain flare-ups.
How Do Sedentary Lifestyle and Obesity Affect Persistent Pain?
A sedentary lifestyle and excess body weight increase mechanical stress on joints and promote systemic inflammation, intensifying pain and accelerating degenerative changes. Deconditioning reduces muscular support and increases injury vulnerability, while inflammatory substances from excess body fat contribute to widespread pain and fatigue. Clinically, initiating small activity goals (e.g., daily walks, physical therapy) can reduce pain sensitivity and improve mood. Combining activity with dietary support and behavioral coaching leads to sustainable improvements.
What Is the Impact of Poor Posture and Repetitive Strain?
Poor posture and repetitive strain cause localized tissue overload, micro-injuries, and chronic pain conditions like tendonopathy or nerve entrapment. Both office and manual laborers face ergonomic risks. Preventive measures include ergonomic assessments, task variation, strengthening, and stretching to balance load and reduce recurrence. Physical therapy and workplace interventions can retrain movement and decrease pain medication needs. Addressing ergonomic issues early prevents acute strain from becoming persistent musculoskeletal pain.
How Can Lifestyle Changes Help Manage Chronic Pain?
Lifestyle changes help manage chronic pain by reducing pain/inflammatory triggers and rebuilding physical capacity/resilience, leading to decreased symptom severity and improved functioning. Graded exercise strengthens structures and counteracts deconditioning; improved sleep and stress management normalize pain modulation. A diet minimizing pro-inflammatory foods, gradual weight loss, and activity pacing support rehabilitation. Integrating these with psychological therapies enhances adherence and yields lasting results.
How Does Dunham House Address Chronic Pain in Dual Diagnosis Treatment?
Dunham House offers integrated residential and outpatient care addressing addiction, mental health, and the psychological factors of chronic pain, using evidence-based and holistic experiential therapies. Our programs emphasize multidisciplinary assessment, trauma-informed approaches, and therapies to improve pain coping and reduce substance use, supporting sustained recovery. Program options (dual-diagnosis, 1-month, 6-month, outpatient) allow for personalized care tailored to individual needs and recovery stages, leveraging our serene campus and experiential therapies for engagement and functional restoration.
What Evidence-Based Therapies Are Used for Chronic Pain and Mental Health?
Evidence-based therapies for dual diagnosis chronic pain include CBT for pain coping, DBT for emotion regulation, mindfulness for arousal reduction, and medication management. These address psychological contributors by reducing catastrophic thinking, enhancing coping, and improving activity adherence. Experiential therapies like Equine-Assisted Learning complement traditional modalities. Integrating these within a trauma-informed framework enhances treatment retention and functional recovery.
How Does a Serene Residential Environment Support Recovery?
A tranquil residential setting minimizes stressors, provides structured routines for sleep and activity, and offers immediate multidisciplinary care, improving pain management and mental health. Nature-focused environments reduce stress, encourage movement, and facilitate experiential therapies. Peer support fosters accountability and models adaptive behaviors. For co-occurring disorders, a balanced environment enhances engagement with long-term recovery.
What Are the Program Options for Individuals with Chronic Pain and Dual Diagnosis?
Integrated centers offer short-term residential care for stabilization, longer-term programs for complex needs, and outpatient programs for ongoing support, allowing for individualized pathways. A 1-month program provides intensive stabilization; a 6-month program supports deeper trauma work and skill development. Outpatient programs facilitate continued therapy and reintegration. For program suitability inquiries, Dunham House welcomes admissions contact via phone and email for guidance.
What Are the Psychological Factors Specifically Contributing to Persistent Neuropathic Pain?
Psychological factors uniquely influence neuropathic pain by modulating central neuroplasticity and inhibitory pathways, altering perceived intensity and disability. Anxiety and depression can reduce natural pain inhibition and increase attention to sensations. Past trauma can sensitize somatic circuits and complicate treatment. Recognizing these drivers supports integrated psychiatric and pain-focused interventions (medication, trauma-informed psychotherapy, rehabilitation) to address mechanisms perpetuating neuropathic symptoms. Subsections explore anxiety/depression effects and trauma-informed care in neuropathic pain.
How Do Anxiety and Depression Exacerbate Nerve Pain?
Anxiety and depression worsen nerve pain by impairing inhibitory pathways and increasing central sensitization, amplifying neuropathic signals for more intense, disabling experiences. Clinically, individuals show heightened vigilance, distress, and activity avoidance, leading to poorer outcomes if mental health isn't addressed. Therapies combine antidepressant/neuromodulating medications with CBT to reframe thinking and encourage activity. Addressing mood disorders alongside neuropathic treatments improves pain control, sleep, and functioning.
What Role Does Trauma-Informed Care Play in Neuropathic Pain Management?
Trauma-informed care applies principles of safety, choice, collaboration, trustworthiness, and empowerment to minimize re-traumatization and enhance treatment engagement for pain influenced by past adverse events. For neuropathic pain, it prioritizes gradual exposure, patient control, and integrated somatic therapies. Trauma screening and adapted interventions can reduce dropout and support effective behavioral/pharmacological treatments. Combining trauma-informed psychotherapy with neuromodulatory strategies addresses psychological and neurobiological factors of persistent nerve pain.
How Can Understanding Fibromyalgia Causes and Symptoms Improve Chronic Pain Treatment?
Fibromyalgia is a chronic pain condition driven by central nervous system mechanisms, characterized by widespread pain, fatigue, sleep disturbances, and cognitive difficulties. Understanding its triggers and symptom patterns guides integrated, multidisciplinary treatment focusing on central pain modulation, activity pacing, and psychological support. Recognizing central sensitization shifts treatment towards graded exercise, sleep normalization, CBT, and central pain processing medications. Early identification can prevent unnecessary procedures and direct care toward restoring function through physical, psychological, and lifestyle strategies. Subsections outline hallmark symptoms and common triggers.
What Are the Key Symptoms of Fibromyalgia?
Fibromyalgia presents with widespread musculoskeletal pain, persistent fatigue, non-restorative sleep, and "fibro fog." These distinguish it from localized pain. Individuals may report increased sensitivity to light, sound, and temperature, and experience flares linked to stress or exertion. Warning signs for urgent evaluation include focal neurological deficits, systemic inflammation, or rapidly progressing symptoms. Recognizing this cluster allows clinicians to prioritize central pain modulation and avoid unnecessary diagnostic testing.
How Do Emotional and Physical Factors Trigger Fibromyalgia Flare-Ups?
Emotional stress, excessive physical exertion, disrupted sleep, and concurrent illnesses commonly trigger fibromyalgia flare-ups by increasing physiological arousal and central sensitization, heightening pain and fatigue. Strategies for managing flares include pacing activities, graded exercise, optimizing sleep, and relaxation/mindfulness. Integrating psychological therapies (e.g., CBT) with physical rehabilitation can decrease flare frequency and support long-term functioning. Multidisciplinary care addressing both emotional and physical triggers yields consistent improvements.
Conclusion
Understanding the complex nature of chronic pain, encompassing its physical and psychological dimensions, empowers you to pursue effective, integrated treatment options. By addressing both pain and mental well-being concurrently, you can achieve improved functioning and a better quality of life through personalized therapies. We encourage you to explore comprehensive care programs that align with your unique needs and challenges. Take the crucial first step toward relief and recovery by contacting a specialized treatment center today.
Dunham House
About Dunham House
Located in Quebec's Eastern Townships, Dunham House is a residential treatment centre specializing in addiction and providing support to individuals with concurrent mental health challenges. We are the only residential facility of our kind in Quebec that operates in English.
Our evidence-based programs include a variety of activities such as art, music, yoga, and equine-assisted therapy. In addition to our residential services, we offer a full continuum of care with outpatient services at the Queen Elizabeth Complex in Montreal.