5 Often‑Missed Signs of Addiction Families Commonly Overlook — How to Recognize Hidden Behavioural, Physical and Emotional Changes
Signs of addiction can develop slowly and be mistaken for stress, ageing or simply a change in personality. Spotting those early changes gives families a chance to act, arranging assessment, connecting with appropriate care for substance use and addressing any co‑occurring mental health needs. This guide breaks down ten commonly missed indicators across behaviour, appearance and mood, links them to likely substances and mental‑health overlaps, and offers clear next steps, including checklists, conversation scripts, symptom-to-substance cues, and guidance on residential and outpatient options.
What Are the Most Overlooked Behavioral Signs of Addiction in Adults?
Behavioural changes can show up long before major medical issues, and they’re often dismissed as personality shifts. Substances alter reward, impulse control and social priorities, and those shifts show up at work, in relationships and in motivation. Recognizing patterns early lets families document what’s happening and prepare an evidence‑based response. Below are subtle behavioural indicators that are frequently missed.
Watch for these behavioural changes:
Gradual withdrawal from social activities: Regularly declining invitations and spending noticeably more time alone without a clear reason.
Inconsistent responsibility: Repeatedly missing deadlines, falling behind on bills, or neglecting everyday tasks they used to manage reliably.
Sudden secrecy about time and money: Unexplained cash shortfalls, vague accounts of where they’ve been, or hidden purchases.
Rapid mood shifts tied to triggers: Sharp highs or lows that seem to follow access to certain people, places or situations linked to substance use.
New or worsening legal or work problems: Small infractions, attendance issues or a drop in performance that did not occur before.
These signs usually appear in clusters rather than alone. If you notice two or more together, begin recording frequency, context and duration , a factual record helps separate a short‑term stress response from a developing substance use disorder and supports a professional assessment.
How Do Subtle Personality Shifts and Mood Swings Indicate Addiction?
Personality shifts and mood instability can be early warning signs because many substances disrupt the brain circuits that regulate emotion and reward. Repeated irritability, increased unreliability or risky choices deserve attention. Note specific examples (dates, settings, duration) to show clinicians how behaviour has changed from baseline , that detail helps distinguish substance-driven changes from primary mood disorders and supports timely, integrated evaluation.
Small, gradual changes, such as losing interest in long‑held hobbies or snapping at small stresses often precede clearer signs and make the issue harder to spot. Pay attention to whether mood shifts happen around particular times or with certain people; when mood instability appears alongside secrecy, financial problems or withdrawal from activities, substance involvement and the need for a dual‑diagnosis assessment become more likely.
Why Is Increased Secrecy and Dishonesty a Hidden Sign of Substance Abuse?
Secrecy often begins as minor omissions and grows as a person protects their use and access. Early clues include vague answers about where they’ve been, changed passwords, unexplained receipts or sudden defensiveness about personal space, behaviours families might dismiss as a desire for privacy. Look for patterns: how often secrecy occurs, in which situations, and whether it lines up with missed responsibilities or mood changes. When secrecy becomes habitual or is paired with fear of discovery, it often reflects efforts to hide activity that carries shame, legal risk or social consequences.
Approach secrecy strategically: gather factual examples before speaking, use neutral, non‑accusatory language, and set predictable boundaries. If clarification attempts trigger denial or escalation, seek a professional assessment to clarify the role of substance use and plan safe, evidence‑based next steps.
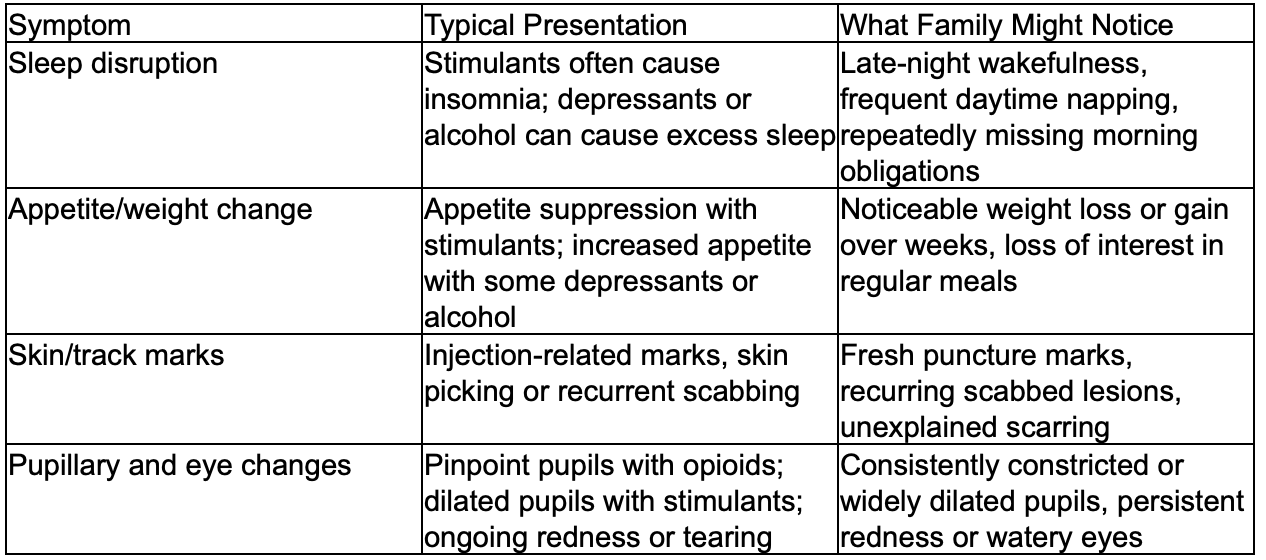
What Hidden Physical Signs of Drug Abuse Should Families Watch For?
Physical changes are often mistaken for illness, stress or normal ageing. Substances can affect sleep, appetite, movement and appearance in recognizable ways; matching observations to likely substance effects helps clinicians assess risk. Below are common physical indicators families sometimes miss and why they matter.
Physical indicators to note:
Neglected grooming or sudden hygiene decline: Less attention to personal care despite the ability to manage it previously.
Persistent sleep changes: New or worsening insomnia, oversleeping, or erratic sleep–wake patterns compared with baseline.
Weight and appetite shifts: Noticeable gain or loss over weeks without an obvious medical cause.
Visible signs of use: Track marks, unusual skin picking, excessive sweating, pinpoint pupils or persistent bloodshot eyes that are dismissed as tiredness.
When these signs persist or appear alongside behavioural changes, document them and seek medical evaluation. A clinician can rule out other causes and, if needed, arrange a focused substance‑use assessment. The table below links common physical symptoms with typical substance presentations and what family members might observe.
Different substances tend to produce distinct physical patterns families can record and report.
Calm, specific reporting of observations increases the chance of a timely and appropriate clinical response.
How Do Unexplained Changes in Appearance and Hygiene Reveal Addiction?
A drop in grooming often reflects shifting priorities, where substance use takes precedence, or it can signal depression or cognitive decline that reduces capacity for self‑care. When grooming slips occur with secrecy, mood swings or declining function, they become stronger indicators of substance involvement. Note when the change began, how it differs from previous habits and any linked behaviours, that factual record is useful for assessment. If hygiene decline leads to social isolation or job loss, it signals functional impairment that should prompt clinical evaluation for substance use and co‑occurring disorders.
Approach the subject gently and without blame: offer practical help with appointments, and express concern rather than shame. If the person resists and decline continues, seek professional guidance on next steps, including medical evaluation for withdrawal risks and referral to evidence‑based treatment.
What Are the Signs of Altered Sleep Patterns and Weight Fluctuations in Addiction?
Many substances directly change appetite and sleep rhythms. Stimulants such as cocaine or methamphetamine typically reduce appetite and fragment sleep, while alcohol and sedatives can cause hypersomnia and, for some people, weight gain. Simple objective records — sleep logs and weight trends, help distinguish short‑lived stress responses from consistent substance‑related effects that matter diagnostically.
If sleep or weight changes occur alongside mood symptoms, cognitive problems or physical signs of use, the likelihood of a substance problem or dual diagnosis increases. Early medical assessment can identify withdrawal risks and other contributors, enabling safer, evidence‑based planning for treatment or referral.
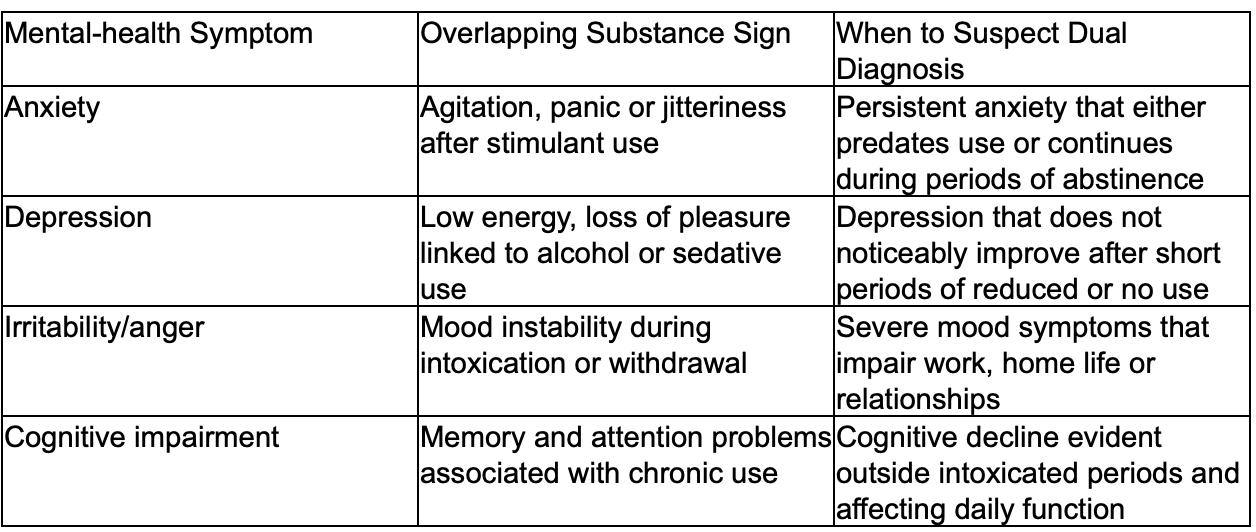
How Can Psychological and Emotional Indicators Signal Dual Diagnosis and Addiction?
Psychological and emotional signs often overlap between substance use disorders and mental health conditions, that overlap is why dual diagnosis (a substance use disorder together with a mental health disorder) is clinically important. When both conditions interact, each can change the course and response to treatment of the other. Spotting overlapping signs, for example, chronic anxiety alongside rising substance use , should prompt families to request an integrated assessment rather than separate or sequential care. Current guidance shows coordinated evaluation and combined treatment improve engagement and reduce relapse risk.
Use the practical mapping below to link common mental‑health symptoms with substance‑related presentations and know when to suspect dual diagnosis.
If emotional symptoms persist despite brief abstinence, seek an integrated assessment so clinicians can map how mental health and substance use interact. Integrated plans combine psychotherapy, medication management and substance‑use interventions rather than treating conditions in isolation.
Dunham House specialises in addiction and concurrent mental health disorders (dual diagnosis). We provide individualised, evidence‑based residential and outpatient care in English on a quiet nature campus in Quebec’s Eastern Townships. Our programmes blend clinical therapies with experiential supports and focus on coordinated, whole‑person care, an approach that improves chances of recovery.
What Role Do Denial and Defensiveness Play in Overlooked Addiction Signs?
Denial and defensiveness are common coping strategies that protect substance use by minimising consequences and blocking help‑seeking, which delays assessment and care. Clinically informed approaches advise families to keep records of concrete examples, use calm, non‑confrontational language, and set clear, consistent boundaries to reduce enabling. If defensiveness escalates to aggression or severe functional decline, seek urgent professional assessment to evaluate safety and treatment needs.
Seeing denial as part of the illness helps families move from moral judgement to practical action: document observations, get clinician support for conversations, and pursue formal referral when appropriate. This structured approach lowers conflict and increases the chance the person will accept help when they are ready.
How Do Increased Anxiety, Depression, and Loss of Interest Relate to Dual Diagnosis?
Anxiety, depression and anhedonia commonly co‑occur with substance use for several reasons: people sometimes self‑medicate distress, substances can trigger or worsen mood disorders, and shared biological and environmental risks increase the chance of both conditions. Clinical guidance emphasises that treating only one condition often fails when both are present. If mood symptoms persist during abstinence or clearly predate substance use, the pattern suggests an independent mental health disorder that needs concurrent treatment.
Integrated care combines therapies such as cognitive behavioural therapy and motivational interviewing with medication management and substance‑use interventions to address both conditions at once. Families should prioritise programmes offering coordinated services because combined care reduces relapse risk and supports better functional recovery over time.
How Can Families Identify and Respond to Overlooked Signs of Addiction?
Responding is easier when families follow a clear, practical process: observe and document, prepare for a compassionate conversation, set and enforce boundaries, and arrange professional assessment when required. Early documentation , dates, concrete behaviours and objective consequences , supports focused conversations and, if needed, clinical referral. The steps below give families immediate actions to move from worry to safe, evidence‑based intervention.
Follow these steps when preparing to respond:
Document concrete examples: Keep a dated log of observable behaviours, missed responsibilities and physical signs.
Choose a calm, non‑judgemental moment: Use “I” statements and stick to specific observations rather than labels.
Set firm, consistent boundaries: State clear supports and consequences, and follow through predictably.
Seek professional assessment: Contact a clinician experienced in dual diagnosis for an integrated evaluation.
Engage family supports: Use trusted allies to reinforce boundaries and help coordinate care logistics.
These steps move families from concern to concrete action and help reduce conflict. Communication scripts and boundary templates can make the first steps easier.
What Are Effective Communication Strategies for Approaching a Loved One?
Clear, non‑blaming communication that uses specific examples and offers help rather than demands increases the chance a loved one will listen. Start with brief factual statements: name the behaviour, describe its impact and express your concern, for example, “I’ve noticed you missed two shifts this month and I’m worried about your health.” Avoid moralising or guessing motives. Offer practical next steps, such as arranging a medical assessment together, and set boundaries in the same conversation so support and accountability go together.
Role‑playing the conversation with another family member or a clinician can refine wording and reduce escalation risk. If the first talk triggers denial or aggression, step back and plan for a professional‑led intervention; experienced clinicians or interventionists can safely facilitate assessment and admissions.
How Can Families Set Boundaries and Encourage Treatment for Addiction?
Boundaries are specific, enforceable rules that reduce enabling and create predictable consequences tied to safety and resources. Examples include limiting financial assistance, requiring participation in assessment to remain in shared housing, or defining visitation rules that protect children and vulnerable household members. Consistency is essential, boundaries without follow‑through lose credibility and can increase harm. Pair boundaries with offers of help: share assessment options, offer to attend appointments, and make supports conditional on treatment engagement when appropriate.
Create a written boundary agreement listing expectations, supports and consequences, and review it with a clinician to address legal and safety issues. Families should also access supports for themselves, therapy, peer groups or clinician consultation , to sustain consistency and avoid burnout.
When families are ready for assessment or referral, Dunham House can help. As a non‑profit residential treatment center specialising in dual diagnosis, we provide individualised, evidence‑based care in English, offering residential and outpatient services. Our team supports families through tailored assessment and referral pathways.
Why Is Understanding Dual Diagnosis Critical When Spotting Hidden Addiction Signs?
Dual diagnosis, the co‑occurrence of a substance use disorder and a mental health disorder — changes how symptoms present and what treatment will be effective. Integrated treatment addressing both conditions together leads to better engagement, lower relapse rates and improved functioning compared with separate or sequential care. Understanding dual diagnosis helps families see why some symptoms persist despite attempts to reduce use and why coordinated care is usually necessary for lasting recovery.
Contemporary guidance supports integrated care teams that coordinate psychotherapy, pharmacotherapy and substance‑use interventions. Below are concise benefits to help families evaluate programme options.
Coordinated clinical planning: Treating both conditions together avoids conflicting approaches.
Reduced relapse risk: Addressing underlying mood or anxiety disorders lowers triggers for substance use.
Improved engagement: Integrated care increases retention and adherence to treatment plans.
How Do Mental Health Disorders Co‑Occur with Substance Use Disorders?
Mental health and substance use disorders often co‑exist because of shared biological vulnerabilities, environmental stressors and self‑medication patterns. Common pairings , for example, anxiety with stimulant misuse or depression with alcohol , are frequent in clinical populations and national surveys. Evidence shows better outcomes when both conditions are treated together. If mood or anxiety symptoms persist outside intoxication or withdrawal, request an integrated assessment so treatment addresses the full clinical picture.
For families, the practical step is to ask clinicians for combined screening for substance use and mental health so the treatment plan targets all contributing factors rather than only the most visible symptoms.
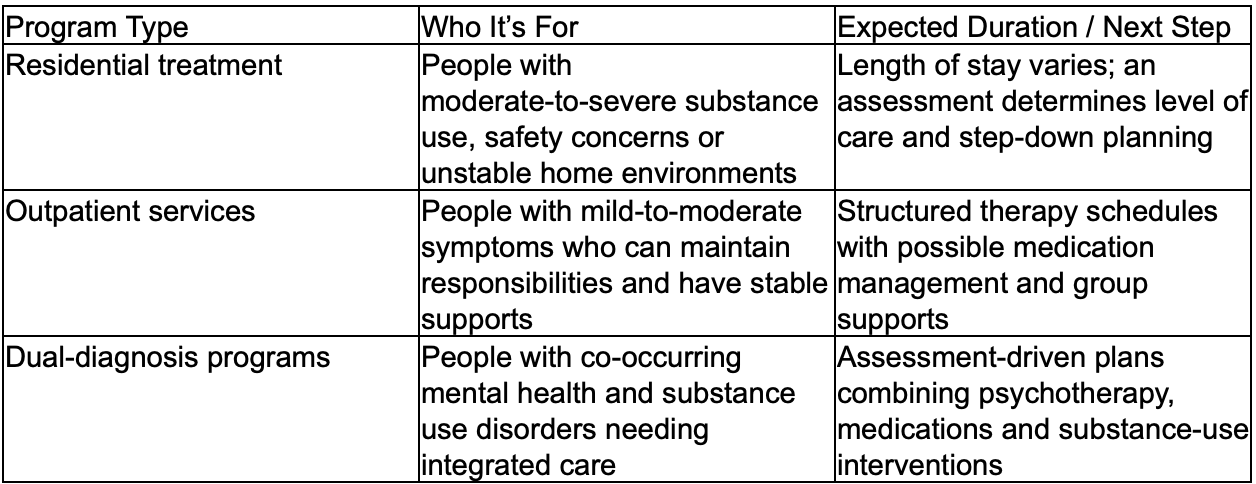
What Are the Benefits of Integrated Dual Diagnosis Treatment Programmes?
Integrated dual diagnosis programmes combine evidence‑based therapies , such as cognitive behavioural therapy for mood and substance issues, with coordinated medication management and recovery supports to treat the whole person. This approach reduces fragmentation, addresses interacting risk factors and supports longer‑term recovery. Compared with sequential or parallel care, integrated programmes show higher engagement and fewer relapses in published reviews.
When reviewing programmes, look for coordinated care teams, individualised treatment plans and options that mix clinical and experiential therapies. Services that combine residential stabilisation with outpatient step‑down care offer continuity and a clearer path through recovery, consistent with best practice.
What Resources and Next Steps Are Available for Families After Recognizing Addiction Signs?
After noticing concerning signs, practical next steps are an integrated assessment, choosing residential versus outpatient care based on severity and risk, and accessing supports for both the individual and the family system. The table below compares programme types to help families choose the right next step and prepare for admissions.
Provide clinicians with concise documentation for admissions: behaviour logs, medical history, current medications and any legal or safety concerns. Clinical teams use this information in triage to determine placement and design an individualised treatment plan.
How Can Families Access Residential and Outpatient Treatment Options?
Access usually begins with an integrated assessment that screens for substance severity, co‑occurring mental health conditions and safety risks. That assessment determines whether residential stabilisation or outpatient supports are most appropriate. Families should gather recent observations, medical details and a short list of current stresses to share at triage. Admissions often require medical clearance, consent forms and information about supports for the transition home. Practical planning for travel, childcare and work leave reduces barriers to engagement.
Dunham House provides residential and outpatient services and guides families through dual diagnosis assessment and admissions. As a non‑profit residential treatment center in Quebec’s Eastern Townships, we offer English‑language, evidence‑based care and support referral coordination and programme selection.
Where Can Families Find Support and Educational Resources for Addiction Recovery?
Families can turn to clinician‑led family therapy, structured education programmes and peer‑led family support groups that focus on boundaries, relapse prevention and caregiver self‑care. Authoritative sources and national guidance documents offer evidence‑based strategies and educational materials to help families understand substance use and co‑occurring mental health conditions. Local clinician networks and community groups, as well as moderated online platforms, provide practical tools and peer connection. A strong support network for caregivers improves a family’s ability to keep boundaries and support the person in care.
Prioritise resources that cover crisis planning, legal protections and how to support recovery without enabling. Engaging professional teams early , during assessment and admission planning — gives families access to clinician‑vetted tools and tailored education for ongoing support.
Start with an integrated assessment: Request combined screening for substance use and mental health to guide placement decisions.
Use family education resources: Attend clinician‑led workshops and peer supports to build consistent boundary‑setting skills.
Plan logistics early: Prepare for admissions by gathering documents and arranging supports at home.
These practical steps reduce delay and help families move from recognition to sustained engagement with appropriate treatment services.
Conclusion
Noticing often‑missed signs gives families the best chance to intervene early. By recognising behavioural, physical and emotional indicators, keeping clear documentation, having compassionate conversations and seeking professional assessment, families can access integrated care for substance use and mental health. Dunham House offers tailored, evidence‑based pathways, explore our resources and reach out when you’re ready; you don’t have to navigate this alone.
Dunham House
About Dunham House
Located in Quebec's Eastern Townships, Dunham House is a residential treatment centre specializing in addiction and providing support to individuals with concurrent mental health challenges. We are the only residential facility of our kind in Quebec that operates in English.
Our evidence-based programs include a variety of activities such as art, music, yoga, and equine-assisted therapy. In addition to our residential services, we offer a full continuum of care with outpatient services at the Queen Elizabeth Complex in Montreal.