Depression and Addiction: Understanding Dual Diagnosis and Effective Treatment Options
What Is Dual Diagnosis and How Common Is It?
Dual diagnosis - often called co-occurring disorders - describes when a person has both a substance use disorder and a mental health disorder (for example, major depressive disorder) at the same time. Understanding how these conditions interact is an important step toward lasting recovery. This article explains the ways depression and addiction influence one another, why integrated treatment improves outcomes, and what practical steps patients, families, and referral sources can take to find coordinated care. Research shows a two-way relationship: depression can lead some people to use substances as a form of self‑medication, while ongoing substance use can deepen depressive symptoms and biological vulnerability. You’ll find clear definitions, context on how common co-occurrence is, typical causes and risk factors, clinical clues that help separate substance-related mood changes from a primary mood disorder, and evidence-based treatment options including psychotherapy and other medication strategies. We also include practical decision tools - checklists for questions to ask programs, side-by-side comparisons of inpatient and outpatient options, and guidance on support groups and relapse prevention - plus recommendations for moving from assessment to treatment planning and when to consider higher-intensity care for safety and recovery support.
What Does Dual Diagnosis Mean in Mental Health and Addiction?
Clinically, dual diagnosis means both a substance use disorder and a mental health disorder meet diagnostic criteria at the same time. Clinicians use a timeline-based evaluation to determine whether depressive symptoms predate substance use, began after substance exposure, or continue during periods of sobriety or medical stabilization. For example, someone may have a long history of recurrent major depression and later develop alcohol dependence, or another person’s low mood may appear primarily during stimulant withdrawal. Identifying these patterns helps clinicians decide whether to prioritize psychiatric stabilization, focused psychotherapy, addiction-specific interventions, or an integrated plan that treats both conditions together.
How Prevalent Are Depression and Addiction Co-Occurring Disorders?
Co-occurrence is common enough to create steady demand for integrated services. Large surveys consistently show higher rates of substance use disorders among people with depressive disorders and, conversely, higher rates of depression among people with substance dependence. Population surveillance indicates that a meaningful share of adults with major depressive disorder will also experience a substance use disorder in their lifetime, while those with substance dependence report elevated rates of persistent depressive symptoms. The practical takeaway: whenever someone presents with either condition, clinicians should screen for the other to reduce missed diagnoses and speed referral to combined care. Awareness of prevalence also helps families and referral sources prioritize dual‑diagnosis screening at intake and in emergency evaluations.
Integrating Treatment for Co-occurring Mental Health Conditions and Substance Use Disorders
Because alcohol use disorder (AUD) and other substance use disorders frequently occur alongside mental health conditions, identifying both problems and treating them together is essential. Individuals with co-occurring conditions are a heterogeneous group: symptom type and acuity, illness severity, chronicity, and recovery capital all influence treatment recommendations. Effective integrated care starts with accurate screening and assessment, then matches treatment intensity and modalities to each person’s needs. This article reviews prevalence, screening tools for AUD and mental health conditions, and approaches to assessing co-occurring disorders - and it outlines models of integrated treatment that address both problems simultaneously.
What Are the Causes and Risk Factors of Dual Diagnosis?
Dual diagnosis typically results from an interaction of biological vulnerability, psychological trauma, and environmental stressors. Genetic and neurobiological factors can raise risk for both mood disorders and substance misuse, while early-life trauma and chronic stress alter brain circuits involved in reward and emotion regulation and can create pathways toward self‑medication. Social determinants , unstable housing, financial strain, limited access to care , increase risk and complicate recovery. During intake, clinicians evaluate this mix of factors to decide whether trauma-informed approaches or higher-intensity services are needed to improve outcomes.
How Do Genetics and Trauma Contribute to Dual Diagnosis?
Genes affect neurotransmitter systems, stress responsivity, and traits like impulsivity that can increase vulnerability to both depression and substance use; a family history often flags this risk. Trauma - especially childhood adversity or other overwhelming events - reshapes stress response systems and raises the likelihood of using substances to blunt intrusive memories or persistent low mood. These forces usually act together: genetic susceptibility sets a baseline risk while traumatic experiences can trigger coping strategies such as substance use, which then further disrupt mood regulation. That combined pathway is why trauma-informed care and careful attention to family psychiatric history are central to thorough dual-diagnosis assessment.
What Role Does Self-Medication Play in Depression and Addiction?
Self‑medication describes using alcohol, opioids, stimulants, or other substances to ease depressive or anxious symptoms. While these substances can bring short-term relief, they often lead to escalation and physiological dependence. Substances can temporarily dampen emotional pain, reinforcing use through negative reinforcement. Over time, brain adaptations strengthen cravings and make stopping harder, and mood symptoms may worsen as tolerance and withdrawal develop. Clinicians look for patterns such as substance use tied to low moods, rapid cycling of mood with substance use cycles, and declining functioning despite negative consequences - all signs that self‑medication is driving the dual-diagnosis dynamic. Addressing self‑medication typically requires integrated behavioral strategies along with pharmacologic support when appropriate to stabilize mood while reducing dependence.
Neurobiological Links Between Depression and Drug Dependence: A Self-Medication Hypothesis
Epidemiological and clinical research documents high comorbidity between depression and drug dependence that may reflect attempts to self-medicate with substances of abuse. Reviews exploring this relationship focus on overlapping neurobiological changes , particularly in reward and motivation circuits , that may underlie core symptoms of both disorders.
What Are the Signs and Symptoms of Co-Occurring Depression and Addiction?
Detecting co-occurring depression and addiction means separating core depressive symptoms from substance-related effects and spotting red flags that both disorders are active. Depressive signs include persistent low mood, loss of interest, changes in appetite and sleep, slowed thinking, and suicidal thoughts. Substance use disorder signs include craving, loss of control, continued use despite harm, tolerance, and withdrawal. Because symptoms overlap (for example, sleep problems or poor concentration), clinicians focus on whether mood symptoms persist during sustained abstinence and on behavioral indicators such as secretive use or social withdrawal that suggest a substance problem. Early identification speeds referral to integrated treatment, reduces medical and safety risks, and strengthens relapse-prevention planning.
How Can You Recognize Symptoms of Depression in Addiction?
To identify depression in the context of substance use, evaluate whether low mood, anhedonia, or suicidal thoughts continue beyond intoxication or acute withdrawal and whether these symptoms independently impair daily functioning. Structured screening tools and clinical interviews help separate substance‑induced mood changes from a primary depressive disorder by tracking timing, duration, and severity relative to substance use. Red flags include persistent hopelessness, marked lack of energy that doesn’t match the substance use pattern, and cognitive problems that don’t resolve after stabilization - all of which warrant psychiatric evaluation and integrated mood-focused treatment. Recognizing persistent depression informs decisions about antidepressant starts, psychotherapy choices, and coordinated medication management with addiction care.
What Are the Signs of Substance Use Disorder in Dual Diagnosis?
Signs that substance use disorder is present alongside depression include increasing preoccupation with obtaining or using substances, unsuccessful attempts to cut down, continued use despite worsening mood or relationships, withdrawal symptoms, and risky behaviors that escalate over time. Functional indicators - missed responsibilities, declining work or school performance, and legal or financial consequences - show that substance-related impairment is clinically significant and needs treatment. Caregivers and referrers should watch for sudden isolation, secretive behavior, or combining medications with alcohol; these raise safety concerns and may prompt urgent assessment. Clear recognition of these signs allows for timely planning that addresses both addiction severity and depressive risk.
What Are the Integrated Treatment Options for Dual Diagnosis?
Integrated treatment addresses depression and addiction together using evidence-based psychotherapy, appropriate medications, and the right level of care. This coordinated approach is the established standard. Effective psychotherapies include cognitive behavioral therapy (CBT) - which targets mood and substance triggers - dialectical behavior therapy (DBT) for emotion regulation, and motivational interviewing to boost engagement. Antidepressant therapy and other appropriate medications are coordinated with behavioral interventions to address biological factors. Levels of care range from inpatient/residential programs that provide medical monitoring to outpatient therapy and partial hospitalization (PHP); the choice depends on severity, safety, and social supports. Integrated teams reduce fragmentation by sharing goals, communicating regularly, and building relapse-prevention plans from the start.
How Does Cognitive Behavioral Therapy Help in Dual Diagnosis Recovery?
Cognitive Behavioral Therapy helps by teaching practical skills to identify and change unhelpful thoughts and behaviors that sustain both depression and substance use. CBT targets relapse triggers through structured skill-building: behavioral activation combats anhedonia, while coping-skills training addresses cravings and high-risk situations. When delivered as part of integrated care, CBT has strong support from clinical trials and practice guidelines for co-occurring depression and substance use disorder. Typical sessions emphasize goal setting, problem solving, and homework that transfers skills into daily life - all designed to strengthen long-term recovery.
What Are Inpatient and Outpatient Dual Diagnosis Rehab Programs?
Inpatient or residential programs provide 24/7 structure, medical management for withdrawal, and intensive therapy when safety or uncontrolled substance use make outpatient care unsafe - appropriate for high-acuity presentations. For instance, facilities like Dunham House specialize in providing comprehensive inpatient dual diagnosis treatment, offering a structured environment for individuals with severe withdrawal risk or complex co-occurring conditions. Outpatient services span weekly therapy to intensive outpatient programs (IOP) or partial hospitalization that deliver several hours of treatment per day while allowing patients to remain at home. The right choice depends on withdrawal risk, medical or psychiatric complexity, available supports, and ability to engage reliably in treatment. Families and referral sources should consider treatment intensity, continuity of psychiatric medication management, and aftercare planning when recommending a program.
If you’re exploring integrated care, arrange an initial clinical assessment with a program that coordinates psychiatric and addiction medicine services. A thorough assessment clarifies needs for psychotherapy, medication, or higher-intensity placement and produces a clear, individualized plan to guide next steps.
How Do You Find the Right Dual Diagnosis Treatment Center?
Choosing the right treatment center means looking closely at clinical depth, staff qualifications, levels of care, and long-term support. For anyone navigating mental health and addiction at the same time, it’s essential to prioritize programs that offer true integrated care, not fragmented services handled in silos.
At Dunham House, a dual-diagnosis inpatient center, treatment is built around collaborative clinical planning. Our addiction specialists and clinical professionals work together from intake to discharge, using standardized dual-diagnosis screening and coordinated medication management for both mood disorders and substance use.
Beyond clinical care, look at real outcomes, alumni support, and the strength of community resources that help sustain recovery long after treatment ends.
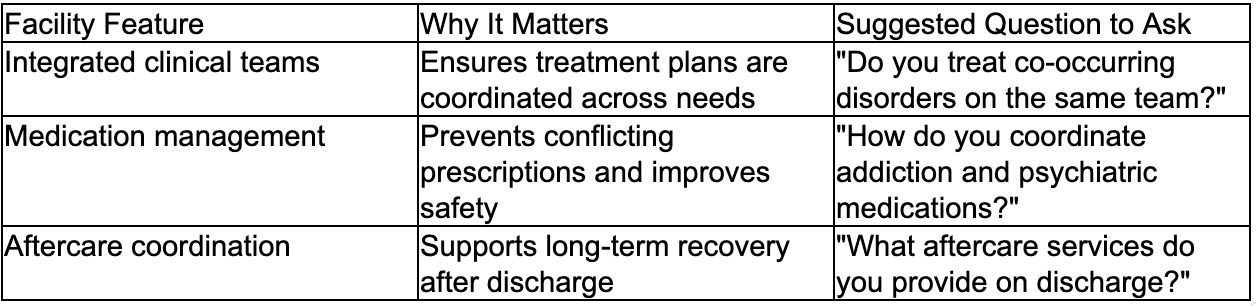
What Questions Should You Ask When Choosing a Treatment Facility?
Use a focused checklist to evaluate integration, clinical credentials, safety practices, and discharge planning. Ask whether the center screens routinely for co-occurring disorders, how the team coordinates between psychiatry and addiction medicine, and what credentialing clinicians hold. Clarify how medication management is coordinated with antidepressant management and how discharge planning supports relapse prevention. Ask about family involvement, peer-support options, and concrete transition steps to outpatient care. These questions help narrow choices to programs ready to manage the complexities of dual diagnosis.
Do you provide integrated treatment for co-occurring depression and substance use disorders? This confirms whether services are coordinated on a single care team.
How do you coordinate medication management between addiction medicine and psychiatry? This addresses safety and continuity of pharmacologic care.
What are your aftercare and relapse prevention plans? This ensures continuity of support after discharge.
Asking these targeted questions helps families and referrers identify programs prepared for complex dual-diagnosis care and supports informed decision-making.
Introductory note: the following facility checklist table summarizes which features matter and suggested questions to ask admissions staff.
Where Can You Access Support Groups and Resources for Co-Occurring Disorders?
Peer-led groups and support networks are a valuable complement to clinical care: they provide community, accountability, and practical coping strategies. Options include 12-step programs, SMART Recovery, and peer-support groups that address co-occurring conditions specifically. National directories and local behavioral-health clinics can point to meetings and peer specialist programs, while clinicians often recommend groups suited to an individual’s needs. When choosing a group, consider whether the setting openly addresses mental health, whether facilitators understand co-occurring disorders, and how the group fits with ongoing clinical care. Peer support works best when it reinforces professional treatment, offers consistent meeting options, and promotes practical relapse-prevention skills.
How Can Individuals Live Well with Dual Diagnosis?
Living well with a dual diagnosis is an ongoing process built on integrated treatment, clear relapse prevention, social supports, and daily self-care that reduces triggers and stabilizes mood. Effective plans typically combine medication adherence, regular therapy or support meetings, learned coping skills for stress and cravings, and safety planning for high-risk times. A written relapse-prevention plan that names triggers, coping steps, emergency contacts, and rapid re‑engagement steps for higher-intensity care lowers the chance of crisis and supports long-term recovery. Lifestyle habits ,consistent sleep, balanced nutrition, regular movement, and meaningful daily activity, strengthen resilience and provide alternatives to substance use, while family involvement and peer support offer accountability and encouragement.
What Strategies Support Recovery and Relapse Prevention?
Concrete relapse-prevention strategies include identifying personal triggers, creating routines that limit exposure to high-risk situations, practicing coping skills from therapy, and keeping regular contact with treatment providers for medication and psychotherapy adjustments. A written plan with early warning signs, coping steps, and emergency contacts helps people act quickly when risk increases; ongoing participation in support groups offers social reinforcement and shared problem solving. Regularly tracking mood and substanc, use patterns, through journaling or structured check-ins , allows early intervention when patterns shift toward relapse. Combining behavioral strategies with medication adherence when prescribed creates a comprehensive approach that addresses both biological and psychological drivers of relapse.
How Can Families Support Loved Ones with Dual Diagnosis?
Families play a crucial role by offering informed, structured support: learn about co-occurring disorders, set compassionate but clear boundaries, and take part in treatment when invited to improve communication and relapse prevention. Helpful actions include helping arrange assessments, attending family psychoeducation sessions, avoiding enabling behaviors, and maintaining caregiver self-care to prevent burnout. Clinicians can guide families on crisis response, encouraging treatment adherence without shame, and knowing when to escalate care for safety. Educated, consistent family support lessens isolation, boosts treatment engagement, and strengthens long-term recovery while protecting family wellbeing.
When ready to move forward, request a clinical assessment that evaluates both depressive symptoms and substance use. An intake team can then recommend the appropriate level of care, explain medication coordination, and outline aftercare supports so families and patients can move from uncertainty to action.
Conclusion
Understanding the interplay between depression and addiction is crucial for effective treatment and recovery. Integrated care not only addresses both conditions simultaneously but also enhances overall well-being and long-term outcomes. If you or a loved one is facing these challenges, consider reaching out for a comprehensive assessment to explore tailored treatment options. Take the first step towards healing by connecting with a dual diagnosis treatment center today.
Dunham House
About Dunham House
Located in Quebec's Eastern Townships, Dunham House is a residential treatment centre specializing in addiction and providing support to individuals with concurrent mental health challenges. We are the only residential facility of our kind in Quebec that operates in English.
Our evidence-based programs include a variety of activities such as art, music, yoga, and equine-assisted therapy. In addition to our residential services, we offer a full continuum of care with outpatient services at the Queen Elizabeth Complex in Montreal.