Addressing the Unique Path: Women's Journey Through Addiction and Recovery
Women's addiction treatment programs are vital for addressing the distinct paths women take to substance use disorders and for cultivating enduring sobriety. This guide delves into the gender-specific biological, psychological, and social factors that shape how addiction manifests in women. We'll explore common co-occurring mental health conditions, highlight the importance of trauma-informed care, identify obstacles to treatment, and showcase the advantages of women-only recovery settings. Additionally, we'll examine the specific impacts of opioids, alcohol, and stimulants on women and illustrate how Dunham House integrates gender-specific and trauma-informed support to achieve better outcomes, encouraging admissions and donations.
How Does Addiction Impact Women Differently Than Men?
Addiction often progresses more rapidly in women, leading to more severe health and psychosocial consequences due to inherent biological vulnerabilities and societal pressures. Recognizing these distinctions allows for personalized interventions that enhance recovery rates and long-term well-being.
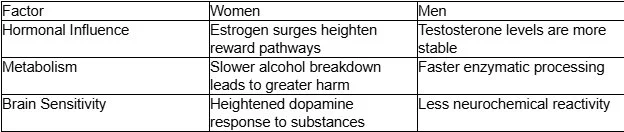
What Biological Factors Influence Addiction in Women?
Hormonal shifts and metabolic variations make women more susceptible to the effects of substances and the severity of withdrawal. The interplay of estrogen and progesterone can intensify cravings and amplify reward responses, while slower alcohol dehydrogenase activity prolongs intoxication and increases the risk of organ damage.
These biological differences emphasize the necessity of gender-responsive protocols that account for hormonal triggers and metabolic risks in recovery planning.
Gender Differences in Drug Addiction: Neurobiological, Social, and Psychological Perspectives in Women – A Systematic Review
A systematic review highlights that women exhibit unique drug use patterns, distinct neurobiological responses, and specific psychosocial challenges in addiction and recovery. Sex hormones like estrogen and progesterone modulate drug sensitivity, leading to faster progression to dependence in women, alongside social and psychological factors such as trauma and caregiving burdens. This research provides a comprehensive overview of the biological, psychological, and social factors that influence addiction differently in women, directly supporting the initial sections of the article.
How Do Psychological and Social Factors Impact Women’s Addiction?
Emotional trauma, the weight of caregiving responsibilities, and societal stigma can increase vulnerability to substance use and discourage individuals from seeking help. Women often turn to substances to self-medicate anxiety or depression in response to life stressors, which can reinforce addictive patterns and lead to isolation from support systems.
Women may use substances as coping mechanisms for past abuse or ongoing domestic violence.
Caregiver duties can delay seeking treatment, resulting in more advanced dependence.
Societal judgment regarding "motherhood" roles can intensify feelings of shame and secrecy.
Addressing these psychosocial triggers through counseling and group therapy helps build resilience and re-establish the supportive connections crucial for recovery.
What Is the Telescoping Effect in Female Addiction?
The telescoping effect refers to the phenomenon where women progress from initial substance use to dependence in a significantly shorter timeframe compared to men. This rapid progression often leads to earlier onset of medical complications, underscoring the urgency of early intervention and specialized screening for women.
A narrative review on alcohol use in women: insight into the telescoping hypothesis from a biopsychosocial perspective
This narrative review examines the telescoping hypothesis in alcohol use disorder among women, noting that biological, psychological, and socio-environmental factors contribute to an accelerated progression to dependence and associated health consequences. Women are more vulnerable to alcohol-related toxicity and often use alcohol to alleviate negative emotions.This research provides an academic perspective on the telescoping effect, specifically in alcohol use among women, and details the biopsychosocial factors contributing to this phenomenon, directly supporting the article's claims.
This effect highlights why "women's rehabs" must offer prompt intake assessments and intensive support to interrupt escalating use patterns before severe dependency takes hold.
How Do Signs of Addiction Manifest Differently in Women?
Signs of addiction in women often present as mood disturbances, social withdrawal, and changes in weight, rather than overt signs of intoxication. Early detection relies on recognizing emotional volatility, increased isolation, or unexplained health complaints alongside substance-related symptoms.
Uncharacteristic mood swings or feelings of depression
Avoiding family gatherings or work responsibilities
Unexplained weight loss or gain
Identifying these more subtle indicators can prompt timely referrals to specialized treatment programs, improving the likelihood of a full recovery.
What Are the Common Co-Occurring Mental Health Disorders in Women with Addiction?
Dual diagnosis, or the co-occurrence of a substance use disorder and another psychiatric condition, is common among women. Integrated care models that address both conditions simultaneously lead to more comprehensive healing and a reduced risk of relapse.
How Does Depression Interact with Substance Use in Women?
Women experiencing depression may self-medicate with alcohol or sedatives, which can worsen mood symptoms and deepen addiction. Effective treatment involves a combination of antidepressant therapy, cognitive restructuring, and relapse prevention strategies to break this self-perpetuating cycle.
What Is the Link Between Anxiety and Addiction in Women?
High levels of anxiety can lead some women to misuse stimulants or benzodiazepines in search of temporary relief, ultimately creating dependency and increasing panic over time. Targeted anxiety management techniques, such as mindfulness-based stress reduction, can help lower substance cravings and improve emotional regulation.
How Does PTSD Affect Women’s Addiction and Recovery?
Post-traumatic stress disorder frequently co-occurs with addiction in women, often stemming from high rates of interpersonal violence and sexual trauma. Trauma-specific therapies like EMDR and dialectical behavior therapy (DBT) can reduce reactivity to triggers, supporting long-term abstinence and an improved quality of life.
What Role Do Eating Disorders Play in Women’s Substance Use?
Eating disorders and substance misuse often share underlying issues related to control, self-image, and emotional regulation in women. Coordinated nutritional counseling and body-positive psychotherapy, alongside addiction treatment, promote holistic recovery.
What Are Effective Integrated Treatment Models for Dual Diagnosis in Women?
Integrated treatment brings together psychiatric care, addiction counseling, and peer support within a single framework. Key components include:
Comprehensive Assessment: A joint evaluation of both mental health and substance use disorders.
Medication Management: Coordinated pharmacotherapy for conditions like depression, anxiety, or PTSD.
Therapeutic Interventions: Concurrent individual, group, and family therapy sessions.
Care Coordination: Case managers ensure smooth transitions between different services.
These integrated models are associated with higher rates of treatment retention and greater improvements in both mental health and sobriety outcomes.
Why Is Trauma-Informed Addiction Care Essential for Women?
Trauma-informed care recognizes the profound impact of past abuse or violence and integrates principles of safety, trust, and empowerment into every facet of treatment. By minimizing the risk of re-traumatization and prioritizing patient agency, this approach fosters deeper engagement and lasting healing.
Why Women Need Trauma-Informed Addiction Care
Research indicates that a high percentage of women in addiction treatment have experienced trauma, with women being twice as likely as men to develop PTSD. Trauma-informed care, which integrates safety, trust, and empowerment, is crucial for improving recovery success rates and reducing relapse by addressing both addiction and underlying trauma.This research underscores the critical link between trauma and addiction in women and the necessity of trauma-informed care, aligning with the article's discussion on co-occurring mental health disorders and the importance of trauma-informed approaches.
What Types of Trauma Commonly Affect Women with Addiction?
Women in recovery frequently report histories of:
Childhood physical or sexual abuse
Domestic violence or intimate partner assault
Traumatic loss or abandonment
Acknowledging and validating these experiences establishes a foundation of safety and trust that is essential for effective counseling.
How Do Trauma-Informed Therapies Support Women’s Recovery?
Therapies such as EMDR, DBT, and somatic experiencing address both the psychological and physiological effects of trauma. These modalities help women to:
Safely process traumatic memories
Develop coping skills for emotional regulation
Rebuild a stable sense of self and personal agency
By incorporating trauma work into addiction programming, women gain the tools they need to resist triggers and prevent relapse.
How Does Addressing Trauma Improve Treatment Outcomes for Women?
Focusing on trauma resolution can significantly reduce relapse rates by addressing a core driver of substance use. Studies indicate that trauma-informed programs can increase treatment retention by up to 30%, enhancing both psychological resilience and long-term sobriety.
What Barriers Do Women Face When Seeking Addiction Treatment?
Women encounter unique obstacles—including stigma, childcare responsibilities, financial limitations, legal concerns, and insufficient support—that can prevent them from accessing care. Overcoming these barriers requires comprehensive solutions tailored to the realities of women's lives.
How Does Stigma Impact Women’s Willingness to Seek Help?
Societal stigma surrounding substance use, particularly for mothers, can create fear of judgment, isolation, and shame. Educational outreach and confidential intake processes can help reduce perceived stigma and encourage earlier engagement with treatment.
What Childcare Solutions Support Mothers in Rehab?
On-site childcare, family therapy, and parenting workshops allow mothers to concentrate on their recovery without jeopardizing their custody. Providing safe, reliable care for children removes a primary barrier to admission.
How Do Financial Challenges Affect Women’s Access to Treatment?
Women are disproportionately affected by poverty and have limited insurance coverage for addiction services. Sliding-scale fees, scholarship programs, and financial counseling can ease economic burdens and make rehabilitation more accessible.
What Legal and Family Considerations Influence Women’s Treatment Decisions?
Concerns about child custody, legal consequences, and family roles can delay the decision to enter treatment. Legal advocacy services and family-inclusive therapy sessions can provide reassurance and promote family healing.
How Can Support Networks Help Women Overcome Treatment Barriers?
A strong support network offers practical and emotional assistance throughout the recovery journey. Support systems can include:
Peer-led recovery groups providing guidance based on lived experience
Mentorship from women who have achieved lasting sobriety
Community partnerships offering housing, job training, and childcare resources
Building these networks enhances resilience and encourages sustained participation in treatment programs.
What Are the Benefits of Gender-Specific Rehab Programs for Women?
Women-only rehabilitation environments create a safe space where shared experiences foster empathy, minimize distractions, and encourage open dialogue. Gender-specific care addresses trauma histories, social roles, and health needs unique to women, leading to improved retention and better outcomes.
How Do Women-Only Rehab Environments Improve Recovery Outcomes?
Eliminating mixed-gender dynamics and potential triggers helps women feel more secure and supported. Research indicates that women-only programs are associated with higher rates of program completion and post-treatment abstinence.
What Types of Gender-Specific Treatment Programs Are Available?
Gender-responsive services encompass a range of options, from residential and outpatient programs to holistic retreats. These may include:
Residential Retreats: Intensive on-site care with 24/7 support.
Outpatient Clinics: Flexible therapy schedules combined with community-based services.
Holistic Centers: Integrative therapies such as yoga, mindfulness, and nutrition counseling.
Each format can be customized to meet women's individual and clinical needs.
How Does Trauma-Informed Care Integrate into Gender-Specific Programs?
Trauma-informed principles are foundational to all therapeutic modalities within female-focused settings. Staff receive specialized training to deliver safe, compassionate care that acknowledges trauma triggers and promotes empowerment.
What Aftercare and Relapse Prevention Strategies Support Women’s Long-Term Recovery?
Continuing care options include alumni groups, peer coaching, and telehealth check-ins. Structured relapse prevention plans incorporate:
Personalized rehearsal of coping skills
Regular attendance at support group meetings
Ongoing mental health services
These measures help solidify gains made during primary treatment and provide protection against relapse.
How Do Specific Substances Affect Women Differently?
Opioids, alcohol, and stimulants interact with women's physiology and life circumstances in ways that can amplify health risks and complicate recovery. Understanding these nuances is crucial for developing precise treatment plans and harm-reduction strategies.
What Are the Unique Effects of Opioids on Women?
Women often experience more intense opioid withdrawal symptoms and a higher risk of overdose due to hormonal interactions and body composition. Buprenorphine-based therapies, calibrated for women's physiology, can reduce withdrawal severity and support stabilization.
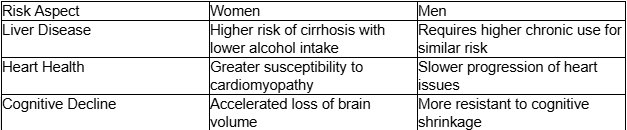
How Does Alcohol Use Differ in Women Compared to Men?
Early screening for alcohol-related harm and gender-tailored detox protocols are essential for safe and effective recovery.
What Are the Gender-Specific Risks of Stimulant Use in Women?
Stimulants can disrupt menstrual cycles, worsen anxiety, and increase cardiovascular strain in women. Therapies focused on stress management and hormonal balance can help minimize relapse triggers.
How Can Dunham House Support Individuals Through Comprehensive and Personalized Addiction Treatment?
Dunham House delivers a fully integrated continuum of care that combines individualized programming with evidence-based therapies, addressing both substance use and mental health in a nurturing environment designed for both men and women.
What Makes Dunham House's Personalized Care Unique?
By offering tailored group curricula and individual therapeutic work, Dunham House fosters peer solidarity and personal empowerment. This approach enhances engagement and reduces dropout rates compared to conventional programs, while recognizing that each individual benefits from personalized therapeutic approaches and peer support dynamics.
How Does Dunham House Address Dual Diagnosis?
An interdisciplinary team of counsellors co-designs treatment plans that treat addiction alongside depression, anxiety, or PTSD. Co-located services ensure seamless care transitions and coherent progress tracking, with treatment approaches adapted to address how mental health conditions may present differently in each individual.
What Family Support Services Does Dunham House Offer?
Comprehensive family therapy sessions, parenting skill workshops, and family support programs enable parents to heal alongside their loved ones. These services preserve family bonds and remove major barriers to treatment entry, supporting both mothers and fathers in their recovery journey.
How Does Dunham House Help Individuals Overcome Stigma and Barriers?
Dunham House emphasizes confidentiality, culturally sensitive staff training, and community outreach to destigmatize treatment. Empowerment groups, peer mentors, and advocacy resources reinforce confidence and reduce external obstacles for all individuals seeking recovery.
By choosing comprehensive, personalized care at Dunham House, individuals find the focused support they need to reclaim their health and build lasting recovery.
Addiction treatment requires a nuanced understanding of individual differences, co-occurring disorders, and personal histories to design effective programs. Personalized, evidence-based approaches remove barriers and optimize outcomes, while specialized therapies for opioids, alcohol, and stimulants cater to each individual's unique needs. Dunham House's integrated model combines these best practices under one roof, offering mental health services and community support that empower both men and women on their journey to sobriety. With comprehensive aftercare and relapse prevention, every person can find the path to sustained recovery and renewed hope.
About Dunham House
Located in Quebec's Eastern Townships, Dunham House is a residential treatment centre specializing in addiction and providing support to individuals with concurrent mental health challenges. We are the only residential facility of our kind in Quebec that operates in English.
Our evidence-based programs include a variety of activities such as art, music, yoga, and equine-assisted therapy. In addition to our residential services, we offer a full continuum of care with outpatient services at the Queen Elizabeth Complex in Montreal.