People Pleasing and Addiction: Understanding, Signs, and Recovery Strategies
People pleasing can morph into a hidden addiction, compelling individuals to set aside their own needs in exchange for fleeting validation and temporary relief. This guide explores how people-pleasing behaviors mirror substance use disorders through compulsive patterns and neural reward pathways. Learn to identify key traits of a people pleaser, recognize the overlap with substance abuse, implement crucial boundary-setting and self-care practices, and choose evidence-based treatments like CBT, DBT, and Schema Therapy.
What Is People Pleasing and How Does It Relate to Addiction?
People pleasing is a behavioral pattern marked by an intense urge to meet others' expectations, functioning much like an addiction by activating reward pathways similar to those triggered by cravings. It often stems from low self-worth and trauma responses, offering brief comfort or approval that reinforces the compulsion. For instance, someone might volunteer for excessive favors to ease anxiety, experiencing a surge of validation that quickly dissipates, prompting them to repeat the behavior.
How Does People Pleasing Function as a Behavioral Addiction?
People pleasing operates as a behavioral addiction by engaging dopamine-driven reward circuits each time external approval is received. The brain learns to associate compliance with positive reinforcement, creating a short-lived high that drives repeated behavior. Over time, tolerance builds, necessitating more extreme accommodation to achieve the same sense of relief. This compulsive cycle mirrors substance use disorder in its pattern of craving-reward-withdrawal and its susceptibility to relapse under stress.
What Is the Role of Codependency in People Pleasing and Addiction?
Codependency describes a relationship dynamic where an individual's sense of self-worth becomes entangled with another person's well-being, reinforcing a people-pleasing addiction. A codependent partner might inadvertently enable substance misuse by covering up consequences or sacrificing their own needs to preserve the connection. This cycle of mutual reinforcement escalates unhealthy behaviors, as the people pleaser gains validation from caretaking, while the individual struggling with addiction relies on that accommodation to continue their substance use.
The Hidden Connection: How People Pleasing Fuels Substance Abuse
People pleasing behaviors significantly increase the risk of developing substance use disorders, with research revealing that individuals exhibiting low agreeableness—a personality trait associated with excessive accommodation of others—face 1.4 to 1.8 times higher odds of substance abuse. This relationship emerges through multiple psychological pathways including emotion dysregulation, social anxiety self-medication, and boundary dysfunction.
The clinical evidence is compelling: 60-80% of individuals with substance-using family members display codependent behaviors, and treatment centers report that 40-60% of clients entering addiction treatment exhibit significant people pleasing patterns. Women show particularly strong correlations between approval-seeking behaviors and substance use.
The psychological mechanisms driving this relationship
Emotion dysregulation serves as the primary pathway connecting people pleasing to substance abuse. A comprehensive meta-analysis of 95 studies involving 156,025 participants found significant relationships between emotion regulation difficulties and substance use (r = 0.19, p < .001). People pleasers struggle most with negative impulse control when experiencing distressing emotions, showing the strongest correlations with substance use (r = 0.38 for multiple substances).
Yeshaia Blakeney, co-founder of Recover Integrity addiction treatment program, describes the clinical pattern: "A lot of people that you find coming into recovery have felt that they've been living for the world and they don't really get theirs. The metaphor for me is like, I do everything I'm supposed to do during the day [for others] and at night, I hide in the closet and drink vodka and smoke meth... that's for me, the rest of its for the world."
Social anxiety and self-medication represent another critical mechanism. National epidemiological data demonstrates that individuals with social anxiety disorder face 2-3 times higher likelihood of developing alcohol use disorders, with 16.4% explicitly endorsing self-medicating with alcohol and drugs.
People pleasing as a powerful risk factor
People pleasing functions as both a predisposing vulnerability and maintaining factor for substance abuse. Boundary dysfunction emerges as a critical risk factor, with clinical research documenting how children who learn their worth depends on pleasing others develop poor internal boundaries.
Dr. Beau A. Nelson, Chief Clinical Officer at FHE Health, explains the trauma connection: "People pleasing can also be a trauma response that is sometimes called 'fawning.' Fawning is a way to avoid a potentially distressing situation recalled from the past, so as to feel safe and mitigate any situation by people pleasing rather than being more assertive."
The conditional self-worth created by approval-seeking behaviors creates specific vulnerabilities. Anne Frazier, a licensed professional counselor in recovery from "addiction to people pleasing," describes: "People pleasing is motivated by lack, where authentic generosity is motivated by abundance. When you're emotionally thirsty and your self-worth is low, you will compromise your own comfort to fill your cup."
Statistical analysis reveals clear risk gradients: individuals scoring in the bottom quartile for agreeableness face odds ratios of 1.4-1.8 for any substance use, 1.6-2.1 for alcohol use disorders, and 2.0-2.8 for illicit drug use.
Evidence-based treatment approaches address both issues
Dialectical Behavior Therapy (DBT) has emerged as the gold standard for treating co-occurring people pleasing and substance use disorders. Originally developed for borderline personality disorder, DBT addresses people pleasing through four core modules: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Multiple clinical trials demonstrate DBT's effectiveness, showing significant reductions in substance abuse among patients with personality disorders.
Cognitive Behavioral Therapy (CBT) modified for people pleasing patterns targets the cognitive distortions underlying approval-seeking behaviors. Treatment components include relapse prevention strategies addressing people pleasing triggers, cognitive restructuring to challenge approval-seeking beliefs, and behavioral experiments to practice boundary setting without guilt.
Treatment outcomes show clear benefits when people pleasing is addressed directly. Research indicates 15-25% better treatment outcomes when personality factors are integrated into addiction treatment, with particular improvements in treatment retention and long-term recovery maintenance.
What Are the Common Signs of People Pleasing and Substance Abuse?
Identifying the overlapping signs of people pleasing and substance abuse requires observing both interpersonal patterns and addictive indicators that contribute to emotional distress.
How Can You Recognize People Pleasing in Daily Life?
Look for consistent patterns where you prioritize others at your own expense:
You agree to favors you later resent and feel drained by.
You apologize preemptively for minor errors or perceived slights.
You second-guess your decisions, fearing disapproval if you choose differently.
You adjust your opinions to align with the group to avoid conflict.
You refrain from expressing your needs, believing they are insignificant.
You experience anxiety or guilt when contemplating declining a request.
You take on others' emotional burdens to maintain smooth relationships.
What Are the Signs of Addiction Linked to People Pleasing?
Signs of addiction intertwined with people pleasing include:
Increasing reliance on external validation to manage emotions, similar to developing tolerance.
Discomfort when asserting boundaries, leading to feelings of guilt or panic.
Loss of control over accommodating impulses, even when it leads to negative personal outcomes.
Excessive time spent focusing on others' needs, detracting from personal responsibilities.
Neglect of hobbies or self-care activities that once brought satisfaction.
These indicators demonstrate how the reward-withdrawal cycle extends beyond social approval into unhealthy dependency.
How Can You Overcome People Pleasing in Addiction Recovery?
Recovering from people pleasing within an addiction framework requires deliberate, structured steps to rebuild self-authority and replace compulsive accommodation with genuine self-care.
What Are the Essential Steps to Break Free from People Pleasing?
Recovery progresses through intentional actions:
Awareness – Pinpoint specific pleasing behaviors and their triggers.
Acceptance – Acknowledge the addictive nature of seeking approval.
Building self-worth – Use affirmations that reinforce intrinsic value.
Exploring boundaries – Clearly define your personal limits in writing.
Assertive communication – Employ "I" statements to express needs directly.
Gradual refusal – Begin by declining small requests to build confidence.
Support network – Share your goals with trusted friends or a sponsor.
Relapse planning – Develop strategies for managing resurfacing guilt or shame.
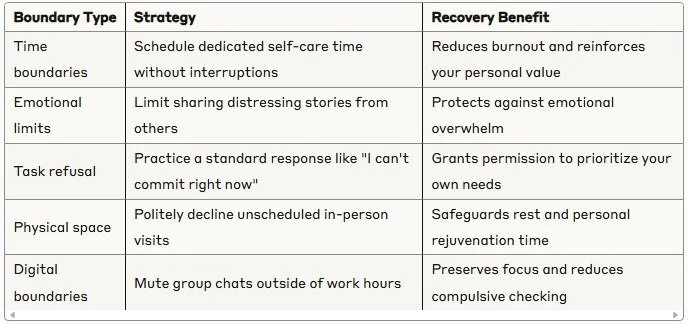
How Does Setting Healthy Boundaries Help in Recovery?
Establishing boundaries empowers individuals to regain control and disrupt addictive approval-seeking loops.
Consistently upholding these limits helps rewire brain pathways away from compulsive caretaking toward healthy self-regulation.
What Therapeutic Approaches Are Effective for People Pleasing and Addiction?
Targeted therapies address both compulsive accommodation and addictive behaviors by reshaping thought patterns, improving emotional regulation, and modifying relational schemas.
How Does Cognitive Behavioral Therapy (CBT) Address These Issues?
Cognitive Behavioral Therapy helps identify distorted beliefs—such as "I'm only valuable if I please others"—and replaces them with balanced self-affirmations. It utilizes structured exercises to challenge automatic thoughts, develop assertive communication skills, and practice gradual exposure to refusal situations. By restructuring cognitive processes and reinforcing healthier behavioral patterns, CBT reduces reliance on external validation and supports relapse prevention.
What Role Does Dialectical Behavior Therapy (DBT) Play in Recovery?
DBT enhances emotion regulation and distress tolerance, equipping individuals with the skills to manage guilt or shame that may arise from setting boundaries. Core DBT modules—mindfulness, interpersonal effectiveness, emotion regulation, and distress tolerance—teach people pleasers to observe urges without judgment and respond with balanced actions. These techniques help break the automatic cycle of panic and compliance, fostering adaptive coping and self-respect.
How Can Schema Therapy Help with People Pleasing and Addiction?
Schema Therapy explores deep-seated life patterns originating in childhood, such as "subjugation" schemas that drive people pleasing. Through experiential exercises and limited reparenting, it addresses unmet emotional needs and helps rewrite maladaptive schemas. By healing the underlying psychological structures that fuel both accommodating behaviors and addictive coping mechanisms, Schema Therapy promotes authentic self-expression and emotional autonomy.
When Should You Seek Professional Mental Health Support?
Professional intervention is recommended when:
Compulsive pleasing significantly interferes with daily life or relationships.
Attempts to decline requests trigger panic attacks or intense guilt.
Addictive behaviors persist or worsen despite self-help efforts.
Co-occurring symptoms of depression, anxiety, or trauma intensify.
You experience thoughts of suicide or significant urges to self-harm.
What Is the Cycle of Shame, Guilt, and Self-Sabotage in People Pleasing and Addiction?
A recurring pattern connects shame, guilt, and the risk of relapse, perpetuating both addictive behaviors and accommodating tendencies.
How Do Shame and Guilt Fuel Addictive Behaviors?
Shame and guilt create intense emotional discomfort that individuals attempt to numb through compliance or substance use. The temporary relief reinforces both the people-pleasing compulsion and addictive consumption, deepening the cycle as self-blame intensifies after each instance of over-accommodation or relapse.
What Is the Role of Resentment in Maintaining People Pleasing?
Resentment accumulates when personal boundaries are repeatedly crossed, yet the people pleaser continues to comply. This suppressed anger further erodes well-being and often resurfaces as self-sabotaging behaviors—avoiding help, isolating, or returning to addictive coping mechanisms—as a way to escape internal conflict.
How Can Awareness of This Cycle Support Recovery?
Understanding the interplay of shame, guilt, and resentment empowers individuals to interrupt automatic responses. By identifying these emotions and employing coping strategies—such as mindful breathing or self-compassion exercises—one can reduce the urgency to appease or numb, paving the way for healthier choices.
People pleasing and addiction can merge into a challenging cycle characterized by compromised authenticity and emotional exhaustion. By recognizing key behaviors, understanding the neurobiological and psychological drivers, and implementing structured recovery steps alongside evidence-based therapies, individuals can reclaim their self-worth and cultivate healthier relationships. Embracing boundary-setting, consistent self-care, and professional support can transform compulsive approval-seeking into empowered autonomy and lasting well-being.
About Dunham House
Located in Quebec's Eastern Townships, Dunham House is a residential treatment centre specializing in addiction and providing support to individuals with concurrent mental health challenges. We are the only residential facility of our kind in Quebec that operates in English.
Our evidence-based programs include a variety of activities such as art, music, yoga, and equine-assisted therapy. In addition to our residential services, we offer a full continuum of care with outpatient services at the Queen Elizabeth Complex in Montreal.
Click here more information about our programs and admissions